
Бесплатный фрагмент - English for Psychotherapy and Counselling: Handbook for Practitioners
Английский для психотерапии и консультирования: практическое руководство
Предисловие
Дорогой читатель, добро пожаловать на страницы этой книги!
Скажу несколько слов, прежде чем перейдем к основной части.
В психологию меня привела моя первая профессия — лингвистика. В прошлом я работала преподавателем и переводчиком английского языка и однажды решила перевести с английского книгу для друзей-психологов, которая была им очень нужна. Впрочем, психологией я увлекалась задолго до этого. Конечно, хотелось понять себя, других и как это все устроено. Однако именно спортивный интерес при переводе поспособствовал тому, что через время я пошла обучаться на психолога-консультанта, преподавателя психологии, а позже — на клинического психолога. Практиковать начала еще во время учебы, и с тех пор психология окончательно стала моей основной сферой деятельности. Собственно, тогда же, когда я проштудировала существующие учебные материалы по английскому для психологов, у меня зародилась идея о создании учебника, пособия или глоссария. Не хватало практикоориентированных материалов, особенно с учетом огромного количества терминов в области психологии и психотерапии, пришедших из англоязычного контекста, и с учетом большого числа непереведенных на русский язык книг психотерапевтической тематики.
Давайте рассмотрим подробнее структуру этой книги и для кого и чем она будет полезна.
Структура
В книге 10 юнитов (или 10 глав). Каждый юнит состоит из следующих секций:
Lead-in — вводная секция, где вы активизируете свои знания, знакомитесь с ключевой темой и настраиваетесь на работу в рамках юнита.
Reading — профессионально ориентированный текст с аутентичной лексикой и примерами.
Vocabulary — работа с ключевыми терминами, выражениями и профессиональными словосочетаниями, необходимыми для понимания и ведения профессионального диалога.
Grammar Focus — изучение грамматических конструкций на материале профессиональных тем, с акцентом на формы и структуры, часто используемые в психотерапевтической практике.
Communication — практика коммуникативных навыков: анализ и разыгрывание типичных профессиональных диалогов, ситуаций из сессий и интервью, развитие языковой гибкости.
Professional Practice — применение изученных структур и терминов в практических заданиях: самопрезентация, описание случаев, упражнения для закрепления профессионального языка.
Vocabulary and Collocations — подборка ключевой лексики юнита и профессиональных устойчивых оборотов с переводом на русский язык для быстрого повторения и удобного использования в работе.
Руководство предназначено для специалистов с уровнем английского языка B1–B2 (Intermediate — Upper-Intermediate). Однако благодаря подробным справочным материалам и структурированной подаче знакомой профессиональной тематики руководство будет интересно также специалистам с уровнем английского A-2 (Pre-Intermediate).
Руководство построено на принципе i+1 (comprehensible input) Стивена Крашена: вы встречаете языковой материал чуть выше текущего уровня, что стимулирует естественное языковое развитие.
Тексты в секции Reading содержат более сложную грамматику и разнообразные структуры, чем изучаемые в секции Grammar Focus. Вы встречаете новые языковые явления в профессиональном контексте, где они понятны благодаря знакомой профессиональной тематике, ключевой лексике из Vocabulary, контексту и предварительной работе в Lead-in.
Руководство следует коммуникативной методике (Communicative Approach), которая лежит в основе всех современных аутентичных курсов английского языка, таких как Headway, New English File, Total English. Это означает, что все материалы юнитов — тексты, задания, инструкции и упражнения — представлены исключительно на английском языке, что создает эффект языкового погружения и помогает развивать способность думать на английском без мысленного перевода. В структуре самого руководства русский язык используется в секции Vocabulary and Collocations в конце каждого юнита, а также в приложениях.
Представленные задания и упражнения могут быть использованы как для групповой, так и для самостоятельной работы.
В конце руководства вы также найдете четыре приложения, которые служат справочными материалами для самостоятельной работы и практики:
Appendix 1. Vocabulary and Collocations — полный список ключевой профессиональной лексики и устойчивых словосочетаний по теме конкретного юнита с переводом на русский язык. Используйте это приложение для быстрого поиска терминов и повторения материала.
Appendix 2. Grammar Reference — справочник по грамматическим темам, изученным в руководстве, с правилами и примерами из профессиональных контекстов. Обращайтесь к нему при выполнении заданий или для систематизации грамматических знаний.
Appendix 3. Therapist’s Phrasebook — набор готовых профессиональных фраз и выражений для различных ситуаций и контекстов в терапевтической практике: от начала сессии до работы с сопротивлением клиента. Есть перевод на русский язык. Этот разговорник поможет вам почувствовать себя увереннее в реальной коммуникации.
Appendix 4. Protocols — образцы протоколов терапевтических сессий с примерами формулировок для документирования работы с клиентами в соответствии с международными стандартами.
Какие задачи поможет решить это руководство?
Это руководство поможет психологу-консультанту, психотерапевту, клиническому психологу решить следующие практические задачи:
В работе с клиентами*:
• Провести первичную консультацию (intake interview) на английском языке
• Собрать анамнез и задать диагностические вопросы с использованием точной профессиональной лексики
• Объяснить клиенту суть терапевтического подхода и техник на понятном английском
• Выстроить терапевтические границы и обсудить условия работы
• Вести протоколы сессий и документировать случаи по международным стандартам
ㅤ
В профессиональном развитии:
• Читать актуальные исследования и профессиональную литературу в оригинале
• Участвовать в англоязычных супервизиях и получать обратную связь от зарубежных коллег
• Представлять клинические случаи (case presentations) на профессиональных встречах
• Участвовать в международных конференциях, семинарах и тренингах
• Проходить дополнительное обучение у международных специалистов без языкового барьера
В повседневной практике:
• Использовать готовые профессиональные фразы для важных моментов сессии (эмпатия, конфронтация, завершение)
• Применять со знанием дела специализированную терминологию психодинамического, когнитивно-поведенческого и экзистенциально-гуманистического подходов
• Понимать культурные особенности профессиональной коммуникации с англоязычными клиентами и коллегами
* Здесь и далее мы будем использовать именно термин “клиент”, а не “пациент”. В англоязычной практике термин “клиент” является общепринятым в консультировании и большинстве направлений психотерапии. Клиент — это активный участник терапевтического процесса, в котором отношения строятся на принципах партнерства и сотрудничества. Поскольку цель руководства – подготовить вас к работе в международной среде, мы будем придерживаться этой терминологической нормы
Для кого будет полезна эта книга?
ㅤ
Практикующие специалисты:
• Психотерапевты и психологи-консультанты, планирующие работать с англоязычными клиентами
• Консультанты, переехавшие в англоязычные страны или работающие онлайн с международной аудиторией
• Клинические психологи, желающие расширить свою практику на англоязычный рынок
• Специалисты, проходящие сертификацию или супервизию у зарубежных коллег
Студенты и обучающиеся:
• Студенты психологических и психотерапевтических программ, готовящиеся к стажировкам за рубежом
• Слушатели программ переподготовки по психотерапии с намерением практиковать на английском
• Психологи, поступающие на магистерские или аспирантские программы в англоязычных университетах
Исследователи и преподаватели:
• Преподаватели психологии, ведущие занятия на английском языке
• Исследователи, публикующие работы в международных журналах
• Специалисты, участвующие в международных конференциях и научных обменах
Специалисты смежных областей:
• Коучи, работающие с психологическими аспектами развития личности
• Специалисты по ментальному здоровью в международных организациях
С большой благодарностью всем моим учителям и близким, которые поддерживали меня на этом пути!
Приятного изучения!
UNIT 1.
INTRODUCTION TO PSYCHOTHERAPY
LEAD-IN:
Mental Health Professionals and Their Roles
Activity 1: What Do You Know?
Look at the list of mental health professionals below and think about the questions:
Mental health professionals:
• Clinical psychologist
• Psychiatrist
• Counselling psychologist
• Psychotherapist
Think about:
• What do you know about each professional? What do they do?
• How are they different? (education, methods, types of problems)
• Which specialist would you recommend for: anxiety, depression, relationship issues, serious mental illness?
Activity 2: Vocabulary brainstorm
Work in small groups. You have 3 minutes to write down as many words as you can related to mental health and therapy.
Example: therapy, counselling, treatment, session, assessment, diagnosis…
Activity 3: Discussion questions
Discuss these questions with your partner:
1. What comes to mind when you hear the word “psychotherapy”?
2. Do you think psychotherapy is different from psychology? How?
3. What do psychotherapists do?
4. What is the difference between a clinical psychologist and other psychologists?
5. Why do people go to therapy?
6. Are there different types of psychotherapy? What do you know about them?
Key vocabulary for this unit:
Match the words with their definitions:
1. Psychology
2. Counselling
3. Psychotherapy
4. Psychiatry
5. Mental health
6. Clinical psychology
a) Medical specialty dealing with diagnosis and treatment of mental disorders
b) The scientific study of the mind and behaviour
c) Treatment using psychological methods through regular interaction
d) Professional guidance to help people cope with specific problems
e) A person’s condition regarding their psychological and emotional well-being
f) Branch of psychology focused on assessment and treatment of mental health disorders
READING:
Mental Health Professionals: Who Does What?
Pre-reading task
Before you read, discuss:
1. What do you think is the main difference between these four professions?
2. What does a clinical psychologist do that other psychologists might not do?
3. Which profession requires medical training?
4. Which focuses on short-term problems?
ㅤ
Mental Health Professionals: Who Does What?
When people experience emotional difficulties, mental health problems, or simply want to understand themselves better, they often wonder: “Who should I see?” The field of mental health includes several types of professionals, and while their work overlaps, there are important distinctions between them.
Psychology is the scientific study of the mind, behaviour, and mental processes. Psychologists are trained professionals who typically hold a doctoral degree (PhD or PsyD) in psychology. They use evidence-based methods to assess, diagnose, and treat mental health conditions. Unlike psychiatrists, psychologists in most countries do not prescribe medication; instead, they focus on psychological interventions and therapy.
Clinical Psychology is a specialized branch of psychology that focuses on the assessment, diagnosis, and treatment of mental health disorders and psychological distress. Clinical psychologists work with individuals, couples, families, and groups to address a wide range of psychological issues, from mild adjustment problems to severe mental disorders such as schizophrenia, bipolar disorder, and severe depression.
What makes clinical psychologists unique is their extensive training in psychological assessment. They are skilled in using various assessment tools, including clinical interviews, behavioural observations, and standardized psychometric tests. A clinical psychologist conducts comprehensive psychological evaluations to understand the nature and severity of a client’s difficulties, considering biological, psychological, and social factors.
Clinical psychologists provide evidence-based psychological therapies and interventions. They work in diverse settings including hospitals, mental health clinics, rehabilitation centers, private practices, universities, and research institutions. Many clinical psychologists also conduct research to develop new treatments and improve existing interventions. Additionally, they often supervise other mental health professionals and contribute to training programs.
The work of a clinical psychologist typically involves:
• Conducting detailed psychological assessments and diagnostic evaluations
• Developing individualized treatment plans based on assessment findings
• Providing various forms of psychotherapy (CBT, psychodynamic, family therapy, etc.)
• Monitoring client progress and adjusting treatment as needed
• Working collaboratively with other healthcare professionals
• Conducting applied research and contributing to evidence-based practice
• Providing clinical supervision to trainees and other professionals
Counselling Psychology is another branch of psychology that shares some similarities with clinical psychology but has a different focus. Counselling psychologists typically work with clients experiencing less severe psychological distress and focus more on personal development, life transitions, and adjustment issues. While clinical psychologists often work with severe psychopathology, counselling psychologists emphasize wellness, growth, and helping people function better in their daily lives.
Counselling (as a profession distinct from counselling psychology) is a helping profession that focuses on specific problems or life transitions. Counsellors, who usually have a master’s degree in counselling or a related field, help clients cope with immediate issues such as career decisions, academic stress, grief, or relationship conflicts. Counselling is typically shorter-term than psychotherapy and more solution-focused. It emphasizes practical coping strategies and goals rather than deep exploration of underlying emotional patterns.
Psychotherapy, often called talk therapy, is a treatment intervention that uses psychological methods through regular personal interaction to help people change behaviour, increase well-being, and overcome problems. While clinical psychologists, counselling psychologists, and counsellors may all provide psychotherapy, the term “psychotherapist” often refers to professionals who engage in more in-depth, long-term therapeutic work. Psychotherapy explores deeper emotional issues, past experiences, and unconscious patterns that influence present behaviour.
Psychiatry is a medical specialty focused on the diagnosis, treatment, and prevention of mental, emotional, and behavioural disorders. Psychiatrists are medical doctors (MDs) who complete medical school followed by specialized training in psychiatry. Because of their medical background, psychiatrists can prescribe medication and may use biological treatments. While some psychiatrists provide psychotherapy, many focus primarily on medication management, especially in contemporary practice where they often work collaboratively with clinical psychologists and other therapists.
Three Main Approaches in Psychotherapy
Within psychotherapy (practised by clinical psychologists and other therapists), three major theoretical approaches have shaped modern practice:
Cognitive-Behavioural Therapy (CBT) is a structured, goal-oriented approach that focuses on the connection between thoughts, feelings, and behaviours. CBT therapists help clients identify negative automatic thoughts and cognitive distortions, then work to challenge and change these patterns. This approach is typically short-term and emphasizes practical homework assignments and skills development. CBT has strong research support for treating anxiety, depression, and many other conditions. Clinical psychologists often use CBT because of its evidence-based effectiveness.
Psychodynamic Therapy has its roots in psychoanalytic theory and emphasizes the role of unconscious processes, early childhood experiences, and relationship patterns. Psychodynamic therapists explore how past experiences shape current behaviour and help clients gain insight into recurring patterns. This approach pays particular attention to the therapeutic relationship itself, including transference (when clients project feelings onto the therapist) and countertransference (the therapist’s emotional reactions to the client). Psychodynamic therapy is usually longer-term than CBT and is often used by clinical psychologists working with complex personality issues and trauma.
Existential-Humanistic Therapy emphasizes personal growth, self-actualization, and the client’s inherent capacity for healing. This approach, which includes person-centered therapy and Gestalt therapy, focuses on the here-and-now experience, authenticity, and the therapeutic relationship. Humanistic therapists provide unconditional positive regard, empathy, and congruence, creating a safe space where clients can explore their feelings and develop self-awareness. Rather than directive techniques, this approach follows the client’s lead and trusts their inner wisdom.
Each approach has its strengths, and many modern clinical psychologists and therapists integrate elements from different schools of thought, practising what is called “integrative” or “eclectic” therapy. The choice of approach often depends on the client’s needs, the assessment findings, and the nature of their difficulties.
Comprehension questions:
1. What is the main educational difference between psychologists and psychiatrists?
2. What makes clinical psychology different from other branches of psychology?
3. According to the text, how does counselling differ from psychotherapy in terms of focus and duration?
4. What is the difference between clinical psychology and counselling psychology?
5. Which professional can prescribe medication? Why?
6. What are the three main approaches to psychotherapy mentioned in the text?
7. Which therapeutic approach focuses on thoughts, feelings, and behaviours?
8. What does “transference” mean in psychodynamic therapy?
9. Which approach emphasizes personal growth and self-actualization? ㅤ
VOCABULARY:
Professional Terminology and Collocations
A. Find words in the text that match these definitions:
1. Based on scientific research and proven methods
(paragraph 2): _______
2. A wide range of psychological issues and conditions that clinical psychologists assess (paragraph 3): _______
3. A complete evaluation of someone’s psychological condition (paragraph 4): _______
4. Tests that measure psychological variables like intelligence or personality (paragraph 4): _______
5. Concentrating on finding practical answers to current problems (paragraph 7): _______
6. Mental processes that happen without our awareness (paragraph 11): _______
7. Inborn, natural, existing from birth (paragraph 12): _______
8. Being genuine and true to oneself (paragraph 12): _______
B. Complete the collocations from the text. More than one answer may be possible:
1. mental health _______
2. psychological _______
3. evidence-_______ methods
4. _______ plans
5. _______ strategies
6. therapeutic _______
7. clinical _______
8. automatic _______
9. personal _______
10. assessment _______
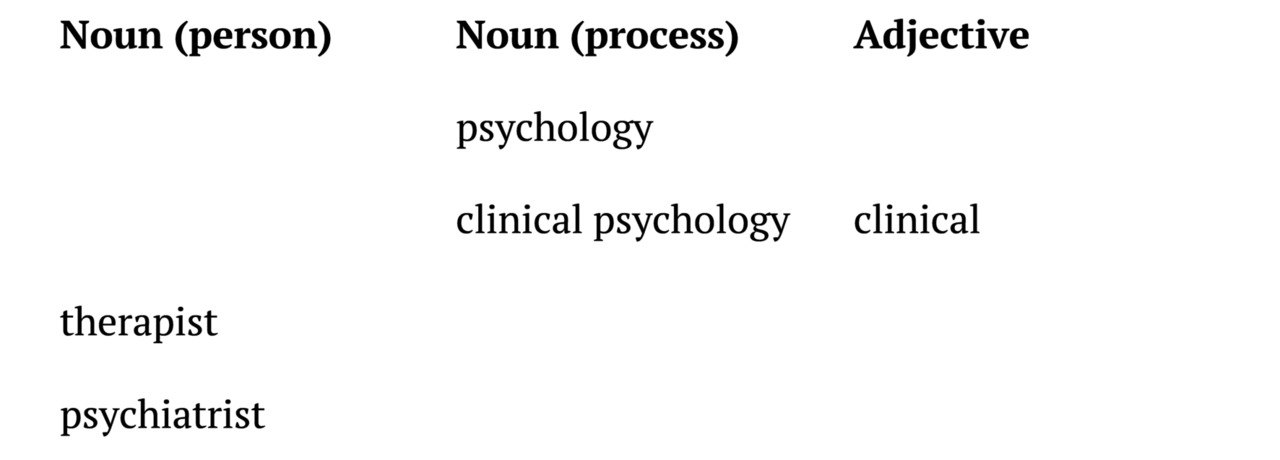
C. Word families
Complete the table:
Discussion questions:
1. In your country, which mental health professional do people usually consult first?
2. What is the role of clinical psychologists in your healthcare system?
3. Do you think the distinctions between these professions are clear in your language?
4. Which therapeutic approach appeals to you most? Why?
5. Should all clinical psychologists be trained in all three approaches, or specialize in one?
6. What are the advantages of seeing a clinical psychologist vs. a psychiatrist?
GRAMMAR FOCUS:
Present Simple for definitions and descriptions / Comparative structures
A. Present Simple for Definitions and Professional Descriptions
We use Present Simple to define concepts and describe what professionals do:
Form:
• Affirmative: Subject + verb (+ s/es for he/she/it)
• Negative: Subject + don’t/doesn’t + main verb
• Questions: Do/Does + subject + main verb?
ㅤ
Examples from Psychology:
• Psychology studies human behaviour and mental processes.
• Clinical psychologists assess and treat mental health disorders.
• Psychotherapists help clients manage emotional difficulties.
• A psychiatrist prescribes medication for mental health conditions.
• Counselling focuses on specific life problems.
ㅤ
Exercise 1: Complete the sentences
Use the correct form of the verb in brackets:
1. Clinical psychologists _______ (assess) mental health conditions using psychometric tests.
2. Psychotherapy _______ (involve) regular communication between therapist and client.
3. Clinical psychologists _______ (not prescribe) medication.
4. _______ (do) clinical psychologists conduct research? Yes, many of them _______ (do).
5. Humanistic therapy _______ (emphasize) personal growth and self-actualization.
6. A counselling psychologist _______ (focus) more on life transitions than severe pathology.
B. Comparative Structures
We use comparative structures to show differences and similarities between concepts:
ㅤ
Structures:
• as + adjective + as (equally)
• more/less + adjective + than
• adjective + -er + than
Examples from Psychology:
• Psychotherapy is more intensive than counselling.
• Clinical psychology is as important as psychiatry in mental healthcare.
• Psychoanalysis is less directive than CBT.
• Clinical psychology training is longer than counselling psychology training.
ㅤ
Exercise 2: Compare the professionals
Complete the sentences using comparative structures:
1. A psychiatrist’s training is _______ (long) than a clinical psychologist’s.
2. Clinical psychologists typically work with _______ (severe) mental health problems than counselling psychologists.
3. A clinical psychologist’s assessment is _______ (detailed) than a counsellor’s initial interview.
4. Counselling sessions are usually _______ (short) than psychotherapy sessions.
5. Clinical psychology is not _______ (medical) as psychiatry.
6. Psychotherapy can be _______ (effective) than medication for some conditions.
7. Clinical psychologists do _______ (much) research than general counsellors.
8. Assessment skills are _______ (important) in clinical psychology than in some other areas.
Exercise 3: Correct the mistakes
Find and correct the mistakes in these sentences:
1. A clinical psychologist are working with complex mental health conditions.
2. Psychiatrist training is more longer than counselling training.
3. Does psychiatrists prescribes medication?
4. A psychotherapist don’t just provide therapy; they also works with emotions.
5. Psychological assessment is as important than medication in clinical practice.
6. What a counselling psychologist do during a first session?
7. Clinical psychologists works in hospitals, clinics, and private practice.
8. Is clinical psychology more scientific than counselling psychology?
9. A counsellor are helping clients with mild to moderate difficulties.
10. Psychiatrists is medical doctors who can prescribe medications.
11. Does a psychotherapist needs a doctoral degree?
12. Counselling psychologists provides talk therapy and don’t diagnose conditions.
COMMUNICATION: Understanding Mental Health Professionals: An Interview with Dr. Sarah Mitchell
Participants: Rebecca Williams (Reporter, Mental Health Today Magazine) and Dr. Sarah Mitchell (Clinical Psychologist, Private Practice)
Reporter: Good morning, Dr. Mitchell. Thank you for agreeing to talk with us today. Our readers are often confused about the differences between mental health professionals. Can you help us understand who does what?
Dr. Mitchell: Of course! I’m happy to clarify. It’s a common confusion, and it’s actually quite important to understand the distinctions.
Reporter: Let’s start with psychiatrists. How are they different from psychologists?
Dr. Mitchell: Well, the main difference is their training and what they can do. Psychiatrists are medical doctors. They go to medical school and can prescribe medication. They focus mainly on the biological aspects of mental health — things like brain chemistry and medications that can help with conditions like depression or anxiety.
Reporter: I see. And what about clinical psychologists? That’s your specialty, right?
Dr. Mitchell: Yes, exactly. Clinical psychologists have a doctoral degree in psychology, not medicine. We can’t prescribe medication, but we’re trained to diagnose mental health conditions and provide therapy. We also do psychological assessments and testing to understand what’s going on with a person’s mental health.
Reporter: So, you both diagnose, but only psychiatrists prescribe?
Dr. Mitchell: Correct. And I should mention counselling psychologists too. They’re similar to clinical psychologists, but they typically work with less severe issues — like relationship problems, stress management, or life transitions. They focus more on helping people with everyday challenges rather than serious mental disorders.
Reporter: That’s helpful. What about psychotherapists? Where do they fit in?
Dr. Mitchell: Psychotherapist is actually a more general term. It can include clinical psychologists, counseling psychologists, and other professionals who provide talk therapy. The key is that psychotherapists use various therapeutic approaches to help people change their thoughts, feelings, and behaviours.
Reporter: Speaking of approaches, can you briefly explain the main types of psychotherapy?
Dr. Mitchell: Sure! There are three major approaches we commonly use. The first is psychodynamic therapy, which comes from Freud’s work. It focuses on unconscious thoughts and how our past, especially childhood, experiences affect us today. It’s often long-term therapy.
Reporter: And the second approach?
Dr. Mitchell: That’s cognitive-behavioural therapy, or CBT. This is very popular today because it’s practical and usually shorter. CBT helps people identify negative thought patterns and change them. The idea is that if you change how you think, you’ll change how you feel and behave. It works really well for anxiety and depression.
Reporter: I’ve heard a lot about CBT, and what’s the third approach?
Dr. Mitchell: The third is humanistic therapy, which includes person-centered therapy. This approach believes that everyone has the potential to grow and solve their own problems. The therapist creates a supportive, non-judgmental environment where clients can explore their feelings and find their own solutions. Carl Rogers developed this approach.
Reporter: So different approaches for different people?
Dr. Mitchell: Exactly. Some people benefit more from exploring their past, others need practical strategies they can use right away, and some just need a safe space to figure things out themselves. Many therapists today actually combine approaches based on what each client needs.
Reporter: That makes sense. One last question — if someone is struggling with mental health issues, how do they know which professional to see?
Dr. Mitchell: Good question! If you think you might need medication, start with a psychiatrist. If you want therapy and psychological testing, a clinical psychologist is a good choice. For relationship issues or life stress, a counselling psychologist or counsellor works well. And remember, many people see both a psychiatrist for medication and a psychologist for psychotherapy.
Reporter: Dr. Mitchell, thank you so much for making this clearer for our readers.
Dr. Mitchell: My pleasure. The most important thing is that people get the help they need, no matter which professional they choose!
ㅤ
TASK 1: True / False / Not Mentioned
Instructions: Read the statements below about the interview. Decide if each statement is:
• TRUE (T) – the statement agrees with the information in the interview
• FALSE (F) – the statement contradicts the information in the interview
• NOT MENTIONED (N/M) – the information is not given in the interview
ㅤ
Statements:
1. Psychiatrists go to medical school and can prescribe medication.
2. Clinical psychologists work only in hospitals.
3. CBT is the oldest approach to psychotherapy.
4. Counselling psychologists typically work with serious mental disorders.
5. Dr. Mitchell has a doctoral degree in psychology.
6. Psychotherapist is another name for psychiatrist.
7. Clinical psychologists can do psychological assessments and testing.
8. Dr. Mitchell thinks medication is more effective than therapy.
9. Psychiatrists focus on the biological aspects of mental health.
10. Psychodynamic therapy focuses on childhood experiences and unconscious thoughts.
ㅤ
Task 2: Personal Response
Discuss: which professional would you prefer to see and why? Which therapy approach sounds most interesting to you?
Task 3: Creating a Comparison Chart
Try to create a visual comparison chart of the four professionals (education, what they can do, typical clients/patients, work settings).
PROFESSIONAL PRACTICE:
Self-Introduction as a Psychology Professional
Sample Introductions
ㅤ
Counselling Psychologist
Hello, my name is Sarah Mitchell, and I’m a counselling psychologist. I work with individuals and couples who are experiencing difficulties in their personal relationships or facing challenging life transitions. My approach focuses on helping clients develop coping strategies and build resilience. I specialize in stress management and career counselling. I’ve been practicing for eight years, and I currently work at a community mental health center. I believe in creating a supportive, non-judgmental environment where clients feel comfortable exploring their concerns.
Psychiatrist
Good morning. I’m Dr. James Chen, a psychiatrist at St. Mary’s Hospital. I assess, diagnose, and treat mental health conditions from a medical perspective. My work involves evaluating patients’ symptoms, prescribing medication when appropriate, and monitoring treatment progress. I specialize in mood disorders and anxiety-related conditions. In addition to medication management, I collaborate with psychologists and therapists to ensure comprehensive care for my patients. I completed my medical degree and psychiatric residency at Johns Hopkins University.
Clinical Psychologist
Hi, I’m Dr. Emma Rodriguez. I’m a clinical psychologist specializing in assessment and treatment of psychological disorders. I conduct psychological evaluations, administer diagnostic tests, and provide evidence-based therapy for individuals with various mental health conditions. My areas of expertise include depression, trauma, and personality disorders. I use cognitive-behavioural therapy and psychodynamic approaches in my practice. I work both in private practice and as a consultant at a local psychiatric hospital.
Psychotherapist
Hello, I’m Michael Thompson, a licensed psychotherapist. I provide talk therapy to help people understand their thoughts, feelings, and behaviours. I work with clients dealing with anxiety, relationship issues, and personal growth challenges. My therapeutic approach is integrative, drawing from humanistic and existential traditions. I’ve been in practice for twelve years and currently see clients in both individual and group therapy settings. My goal is to help people gain insight and make meaningful changes in their lives.
ㅤ
Useful Phrases for Self-Presentation
Stating Your Name and Title
• My name is…, and I’m a…
• I’m Dr./Mr./Ms. …, a licensed/qualified…
• You can call me… I work as a…
Describing Your Role
• I specialize in…
• My main focus is…
• I work with clients/patients who…
• My area of expertise is…
• I primarily deal with…
Explaining Your Approach
• I use/practice…
• My approach is based on…
• I combine… with…
• I believe in…
• My therapeutic style is…
Mentioning Your Experience
• I’ve been practising for… years
• I have… years of experience in…
• I completed my training at…
• I previously worked at/as…
Describing Your Work Setting
• I work at/in…
• I’m currently based at…
• I maintain a private practice in…
• I see clients both in… and…
Highlighting Your Goals
• My goal is to help clients…
• I aim to support people in…
• I focus on helping patients…
• I work towards…
ㅤ
Practice Exercises
ㅤ
Exercise 1: Complete Your Introduction
Fill in the blanks with information about yourself to create your own professional introduction.
Hello, my name is __________, and I’m a __________. I work with __________ who are experiencing __________. My approach focuses on __________. I specialize in __________. I’ve been practising/studying for __________, and I currently work/study at __________. I believe in __________.
Exercise 2: Match and Complete
Match the sentence starters with appropriate endings, then write three sentences about yourself.
Sentence starters:
• My main focus is…
• I’ve been practising for…
• My therapeutic approach is based on…
• I work with clients who…
• My goal is to help…
Possible endings:
• ...are struggling with anxiety and stress
• ...cognitive-behavioural principles
• ...supporting people through difficult transitions
• ...five years in various clinical settings
• …working with children and adolescents
Exercise 3: Build Your Introduction (Step-by-Step)
Write one sentence for each category to build your complete introduction:
1. Name and title: _________________________________
2. Who you work with: _________________________________
3. Your specialization: _________________________________
4. Your approach/methods: _________________________________
5. Your experience/education: _________________________________
6. Your workplace: _________________________________
7. Your professional philosophy: ______________________________
ㅤ
Exercise 4: Listening and Note-Taking
Listen to your partner’s introduction and complete the information:
• Name and title: _________________________________
• Specialization: _________________________________
• Type of clients: _________________________________
• Approach/methods: _________________________________
• Experience: _________________________________
• Current workplace: _________________________________
Vocabulary and collocations for Unit 1
psychology — психология
counselling — консультирование
psychotherapy — психотерапия
psychiatry — психиатрия
mental health — психическое здоровье
clinical psychology — клиническая психология
clinical psychologist — клинический психолог
psychiatrist — психиатр
counselling psychologist — психолог-консультант
psychotherapist — психотерапевт
emotional difficulties — эмоциональные трудности
mental health problems — проблемы психического здоровья
mental health professionals — специалисты по психическому здоровью
evidence-based methods — методы, основанные на научных данных
prescribe medication — назначать лекарства
psychological interventions — психологические вмешательства/интервенции
mental health disorders — расстройства психического здоровья
psychological distress — психологический дистресс
adjustment problems — проблемы адаптации
severe mental disorders — тяжелые психические расстройства
psychological assessment — психологическая оценка
assessment tools — инструменты оценки
clinical interview — клиническое интервью
behavioural observations — поведенческие наблюдения
psychometric tests — психометрические тесты
comprehensive psychological evaluation — всесторонняя психологическая оценка
mental health clinics — клиники психического здоровья
rehabilitation centers — реабилитационные центры
private practice — частная практика
treatment plans — планы лечения
assessment findings — результаты оценки
monitor client progress — отслеживать прогресс клиента
adjust treatment — корректировать лечение
healthcare professionals — медицинские специалисты
clinical supervision — клиническая супервизия
personal development — личностное развитие
life transitions — жизненные переходы
adjustment issues — проблемы адаптации
cope with — справляться с
relationship conflicts — конфликты в отношениях
coping strategies — стратегии совладания
solution-focused — ориентированный на решение
underlying emotional patterns — скрытые эмоциональные паттерны
psychological methods — психологические методы
change behaviourehavior — изменить поведение
increase well-being — повысить благополучие
overcome problems — преодолеть проблемы
unconscious patterns — бессознательные паттерны
biological treatments — биологические методы лечения
negative automatic thoughts — негативные автоматические мысли
cognitive distortions — когнитивные искажения
unconscious processes — бессознательные процессы
childhood experiences — детские переживания
relationship patterns — паттерны отношений
gain insight — обрести/получить инсайт
therapeutic relationship — терапевтические отношения
transference — перенос
countertransference — контрперенос
personal growth — личностный рост
self-actualization — самоактуализация
inherent capacity — врожденная способность
unconditional positive regard — безусловное позитивное принятие
self-awareness — самосознание
authenticity — аутентичность
psychopathology — психопатология
mental health condition — состояние психического здоровья
UNIT 2.
FIRST CONTACT AND BUILDING RAPPORT
LEAD-IN:
First Impressions and Creating a Safe Space
Activity 1: First Impressions Matter
Think about your own experiences. Reflect individually for 2 minutes, then share with a partner:
• What makes you feel comfortable when meeting someone new in a professional setting?
• Can you remember a time when someone made you feel welcome immediately? What did they do?
• What might make a person feel nervous about meeting a psychologist for the first time?
• How quickly do you form an impression of a new person? Do first impressions change?
Activity 2: Creating a Safe Space
Work in small groups. Look at these scenarios and discuss: Which therapist behaviours help build trust? Which might create barriers?
Scenario A: The therapist greets the client warmly, offers them a choice of where to sit, and begins by saying, “I’m glad you’re here. Take your time to settle in”.
Scenario B: The therapist immediately starts asking detailed questions about the client’s problems without any introduction.
Scenario C: The therapist explains what will happen in today’s session and checks if the client has any questions before beginning.
Scenario D: The therapist talks extensively about their own qualifications and achievements.
Activity 3: Think-Pair-Share
Think (1 minute): What questions might a client have when they first meet a psychologist?
Pair (3 minutes): Share your ideas with a partner and add to your list.
Share (5 minutes): Groups share with the class. Create a master list on the board.
Key vocabulary for this unit:
Match the words with their definitions:
1. Rapport
2. Therapeutic alliance
3. Confidentiality
4. Boundaries
5. Informed consent
6. Safe space
a) The agreement to protect private information shared in therapy
b) Professional limits that define the therapeutic relationship
c) A trusting connection between therapist and client
d) Permission given by a client after receiving full information about treatment
e) The collaborative relationship between therapist and client working toward goals
f) An environment where a client feels comfortable expressing themselves
READING:
The First Meeting with a Client: Building Trust and Therapeutic Alliance
Pre-reading task
Before you read, discuss with a partner:
1. What do you think happens in the first therapy session?
2. What information should a therapist provide for a new client?
3. How might a client feel during their first meeting with a psychologist?
4. What makes a good first impression in a professional helping relationship?
ㅤ
The First Meeting with a Client: Building Trust and Therapeutic Alliance
The initial therapy session is unlike any other professional encounter. For the client, it often represents a significant step — one that may have taken weeks or months of consideration before they finally picked up the phone to make an appointment. Many clients arrive feeling anxious, uncertain, or vulnerable. They may be wondering: “Will this person understand me? Can they really help? What if I’m judged?” For the therapist, the first session is an opportunity to create a foundation of trust and safety that will support all future therapeutic work.
Creating the Right Environment
The first impression begins before any words are spoken. Research shows that the therapeutic alliance — the collaborative relationship between therapist and client — is often established in the first session and remains stable throughout treatment. This means that what happens in the initial meeting matters tremendously.
When greeting a new client, warmth and professionalism are equally important. A therapist typically welcomes the client in the waiting area, makes eye contact, offers a warm greeting, and invites them to follow to the therapy room. Some therapists offer a brief tour, which helps the client orient themselves and reduces anxiety. Simple gestures like offering the client a choice of where to sit can give them a sense of control and comfort.
The therapy room itself should feel safe and private. Comfortable seating, appropriate lighting, and the absence of distractions all contribute to creating what therapists call a “safe space” — an environment where clients feel they can speak freely.
The Opening Conversation
Once seated, the therapist typically begins by acknowledging that first sessions can feel uncomfortable. A statement like, “I know it can feel strange talking to someone you’ve just met about personal matters. That’s completely normal, and we’ll take things at your pace,” can immediately reduce anxiety.
Before diving into the client’s concerns, the therapist explains what will happen during this first session. This might sound something like: “Today, we have about 50 minutes together. We’ll spend some time going over important information about confidentiality and how therapy works, and then I’d like to hear from you about what brings you here. Do you have any questions before we begin?”
Informed Consent and Confidentiality
A critical component of the first session is discussing informed consent. This isn’t just a legal formality — it’s an ethical cornerstone that empowers clients and establishes transparency. Informed consent means ensuring the client fully understands what they’re agreeing to before therapy begins.
The therapist explains several key elements:
The nature of therapy: What therapy involves, the approaches the therapist uses, and what clients can generally expect from the process.
Confidentiality: Everything discussed in therapy remains private and confidential. This principle is essential because clients need to trust that their information is safe in order to speak openly. However, there are important limits to confidentiality that must be clearly explained:
• If the client is at risk of harming themselves
• If the client is at risk of harming someone else
• If there is suspected abuse or neglect of a child, elderly person, or dependent adult
• If records are subpoenaed by a court
• If the client provides written permission to share information
Most therapists say something like: “What we discuss here is confidential, which means I won’t share this information with anyone without your permission. However, there are a few exceptions where I’m legally required to break confidentiality, particularly if there’s a risk of harm to you or someone else. Does that make sense? Do you have any questions about confidentiality?”
Risks and benefits: while therapy is generally beneficial, it can sometimes be uncomfortable as clients explore difficult emotions or memories. The therapist discusses both potential benefits and any risks.
Practical matters: this includes session frequency, length, fees, cancellation policies, and what to do in case of emergency.
Client rights: clients have the right to ask questions, refuse any intervention, seek a second opinion, and end therapy at any time.
While many therapists provide written consent forms, the verbal discussion is equally important. The therapist should invite questions and check for understanding throughout this explanation.
Establishing Therapeutic Boundaries
Boundaries are the professional limits that define the therapeutic relationship. Clear boundaries create safety and help clients know what to expect. Boundaries are established from the very first contact and are maintained throughout treatment.
Therapeutic boundaries include:
• Session structure (length, frequency, location)
• Contact between sessions (whether clients can call or email, and under what circumstances)
• Social media policies (most therapists maintain strict boundaries around social media connections with clients)
• Physical boundaries (professional, appropriate physical space)
• Role clarity (the therapist is not a friend, but a trained professional providing treatment)
Boundaries are not meant to be cold or distant. Rather, they create a consistent, safe framework within which the therapeutic relationship can develop. Good boundaries actually build trust because clients learn that the therapist is reliable, consistent, and professionally committed to their wellbeing.
Building Rapport
Once the administrative matters are addressed, the therapist invites the client to share their story. This is typically done with an open-ended question such as, “What brings you to therapy at this time?” or “Tell me a bit about what’s been going on for you”.
Building rapport — a sense of connection and trust — is the primary goal of the first session. The therapist does this through:
• Active listening: giving full attention, avoiding interruptions, and showing through body language that they’re engaged
• Empathy: trying to understand the client’s experience from their perspective
• Unconditional positive regard: accepting the client without judgment
• Validation: acknowledging the client’s feelings and experiences as real and understandable
• Appropriate self-disclosure: occasionally sharing relevant professional experiences (but keeping the focus on the client)
Research consistently shows that the quality of the therapeutic relationship is one of the strongest predictors of positive therapy outcomes. A strong therapeutic alliance means the therapist and client are working together collaboratively toward agreed-upon goals.
Collaborative Goal-Setting
Toward the end of the first session, the therapist and client begin discussing goals. What does the client hope to achieve through therapy? What would improvement look like for them? This collaborative goal-setting ensures that therapy is focused and meaningful.
The therapist might ask, “If our work together is successful, what will be different in your life?” or “What would you like to focus on first?”. These goals provide direction and help both therapist and client track progress over time.
Closing the First Session
As the session draws to a close, the therapist typically summarizes what has been discussed. This might include acknowledging the main concerns the client has shared, highlighting any strengths noticed, and outlining the next steps.
The therapist provides encouragement, recognizing the courage it takes to seek help. They discuss the frequency of future sessions and schedule the next appointment. Many therapists also check in about how the client is feeling: “How are you feeling about our meeting today? Do you have any questions or concerns?”.
The goal is for the client to leave the first session feeling heard, hopeful, and clear about what to expect moving forward. While one session cannot solve all problems, a strong first meeting creates the foundation for meaningful therapeutic work to come.
Comprehension Questions
1. According to the text, why do many clients feel anxious before their first therapy session?
2. Why is the first impression so important in therapy?
3. What is a “safe space” and why is it important?
4. What are the main elements that therapists explain during informed consent?
5. What are the limits to confidentiality that therapists must explain?
6. How do therapeutic boundaries help clients?
7. What are the ways to help therapists build rapport with new clients?
8. What is the therapeutic alliance and when is it typically established?
9. Why is collaborative goal-setting important in the first session?
10. What should happen at the end of the first session?
VOCABULARY:
Rapport, Boundaries, and Therapeutic Relationship Terms
A. Find words or phrases in the text that match these definitions:
• Easily hurt physically or emotionally (paragraph 1): _______
• The person receiving therapy (used throughout): _______
• Agreement and permission based on full information
(paragraph 5): _______
• The quality of being open and honest (paragraph 5): _______
• Listening with full attention and engagement
(paragraph 11): _______
• Understanding and sharing another person’s feelings
(paragraph 11): _______
• Acceptance without criticism (paragraph 11): _______
• Working together toward a common goal
(paragraph 13): _______
ㅤ
B. Complete the collocations from the text:
1. therapeutic _______
2. _______ spaces
3. informed _______
4. _______ consent
5. build _______
6. establish _______
7. _______ listening
8. open-_______ question
9. _______ regard
10. collaborative _______-setting
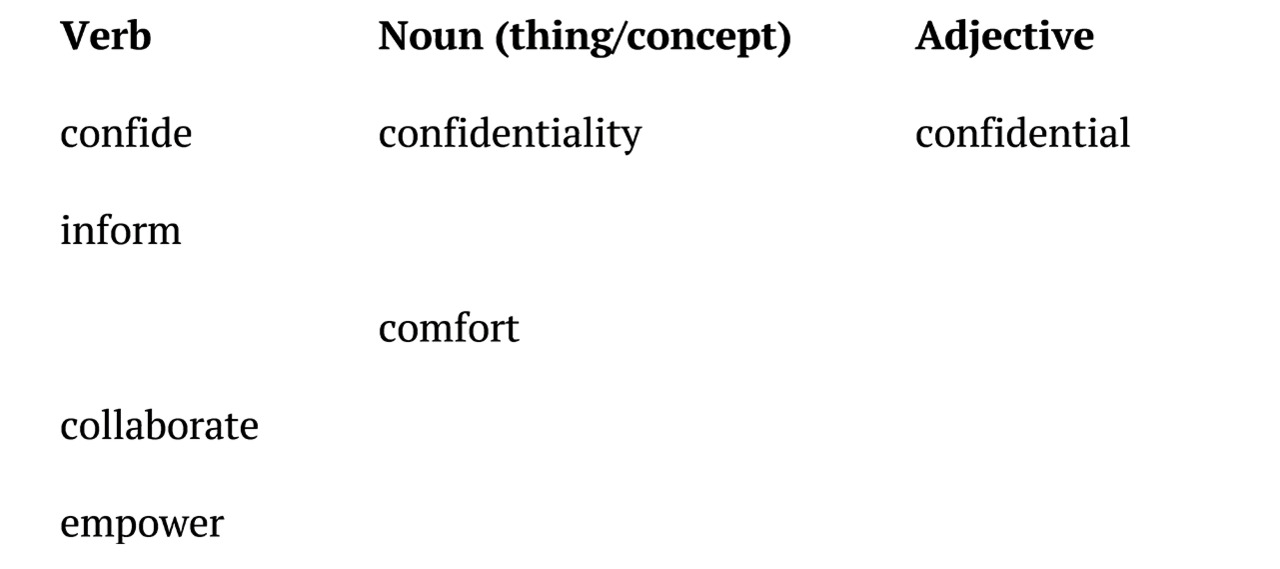
C. Word families
Complete the table:
D. Vocabulary in context
Choose the correct word to complete each sentence:
1. The therapist showed great _______ (empathy / sympathy) by truly understanding the client’s perspective.
2. Clear _______ (borders / boundaries) help create a safe therapeutic environment.
3. The client felt _______ (vulnerable / week) sharing such personal information.
4. Therapists must _______ (establish / install) trust from the very first meeting.
5. The _______ (relationship / rapport) between therapist and client developed quickly.
6. _______ (Informed / Knowledgeable) consent ensures clients understand the therapy process.
7. The therapist practised _______ (active / busy) listening throughout the session.
8. Setting _______ (collaborative / collective) goals helps focus the therapy work.
GRAMMAR FOCUS:
Present Simple vs. Present Continuous / Question Formation
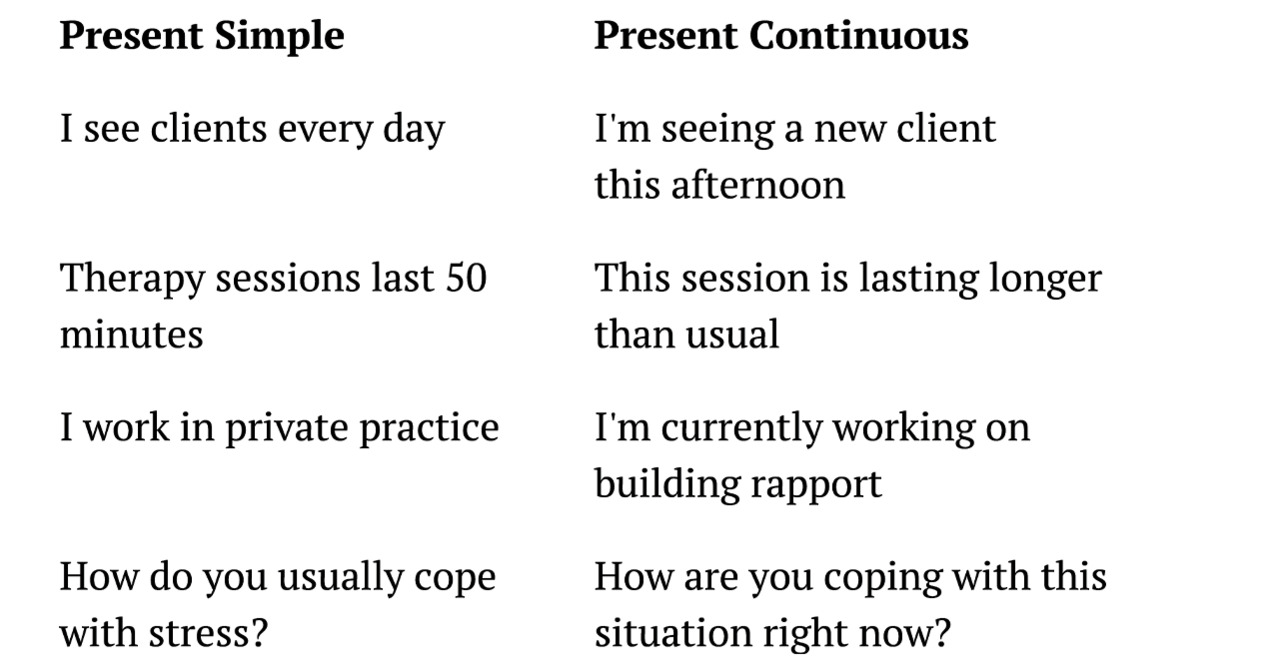
A. Present Simple vs. Present Continuous
We use different tenses to describe different types of actions in therapy:
Present Simple:
• For regular routines, permanent situations, and general truths
• For describing what professionals generally do
Form:
• Affirmative: Subject + verb (+ s/es for he/she/it)
• Negative: Subject + don’t/doesn’t + main verb
• Questions: Do/Does + subject + main verb?
Examples from therapy practice:
• Therapists explain confidentiality in the first session.
• I work with clients on Mondays and Wednesdays.
• Clinical psychologists don’t prescribe medication.
• Do you feel comfortable discussing this topic?
Present Continuous:
• For actions happening now, at this moment
• For temporary situations
• For describing what is currently happening in a session
Form:
• Affirmative: Subject + am/is/are + main verb-ing
• Negative: Subject + am/is/are + not + main verb-ing
• Questions: Am/Is/Are + subject + main verb-ing?
Examples from therapy practice:
• I am listening carefully to what you’re saying right now.
• The client is describing their recent experiences.
• We are working together to identify your goals today.
• Are you feeling anxious at this moment?
Key differences in therapeutic context:
Exercise 1: Choose the correct tense
Complete the sentences with the correct form of the verb in brackets:
1. In our first session, we typically _______ (discuss) what brings you to therapy.
2. Right now, I _______ (explain) how confidentiality works.
3. Most therapy sessions _______ (last) between 45 and 60 minutes.
4. At this moment, the client _______ (share) very personal information.
5. Clinical psychologists _______ (assess) clients using various methods.
6. I _______ (listen) carefully to what you _______ (say).
7. We _______ (not make) major decisions in the first session.
8. _______ you _______ (feel) comfortable talking about this now?
9. Therapists _______ (build) rapport from the very first meeting.
10. I _______ (think) about what goals we should focus on.
Exercise 2: Correct the mistakes
Find and correct the mistakes in these sentences:
1. I’m usually working with adolescents and young adults.
2. Right now, I explain the limits of confidentiality to my client.
3. Are you understanding what I’m saying about boundaries?
4. The therapeutic relationship is building over time.
5. What do you feeling about starting therapy?
6. I’m believing that the first session is very important.
7. We are typically discussing informed consent at the beginning.
8. The client is seeming nervous in every first session.
9. Do you currently experiencing any major stressors?
10. I work on establishing rapport with you at this moment.
ㅤ
B. Question Formation in Therapy
Asking the right questions is essential for building rapport and gathering information. In therapy, we use both closed questions (yes/no answers) and open-ended questions.
Closed Questions (Yes/No):
• Present Simple: Do/Does + subject + main verb?
• Present Continuous: Am/Is/Are + subject + verb-ing?
• Present Perfect: Have/Has + subject + past participle?
Examples:
• Do you feel ready to start therapy?
• Are you experiencing anxiety right now?
• Have you been in therapy before?
Open-ended Questions (encourage detailed responses):
Use question words: What, Where, When, Why, How, Who
Examples:
• What brings you to therapy today?
• How are you feeling about being here?
• What would you like to achieve through therapy?
• How do you usually cope when things are difficult?
• What made you decide to seek help at this time?
Exercise 3: Form questions
Create appropriate questions for a first therapy session using the prompts:
1. (you / ever / see / therapist before)
_______________________________?
2. (what / bring / you / here today)
_______________________________?
3. (how / you / feel / right now)
_______________________________?
4. (you / have / any questions / about confidentiality)
_______________________________?
5. (what / you / hope / achieve / through therapy)
_______________________________?
6. (how long / you / experience / these difficulties)
_______________________________?
7. (you / feel / comfortable / talking about this)
_______________________________?
8. (who / know / that you / come / therapy)
_______________________________?
Exercise 4: Open or Closed?
Identify whether these questions are open or closed. Then, rewrite the closed questions as open questions:
1. Do you have a support system? __________
2. What does your support system look like? __________
3. Are you sleeping well? __________
4. Have you thought about your goals for therapy? __________
5. What brings you here today? __________
6. How are you managing stress? __________
7. Is this situation affecting your relationships? __________
8. Do you want to tell me more about that? __________
COMMUNICATION:
Intake session
Setting: Dr. Maria Santos, a clinical psychologist, is meeting her new client, Robert, for the first time. Robert is a 28-year-old man who has been experiencing anxiety.
Part 1: The Greeting and Opening
Dr. Santos: Hello, Robert? I’m Dr. Santos. It’s nice to meet you.
Robert: Hi. Nice to meet you too.
Dr. Santos: Please, follow me. My office is just down this hallway. (They walk to the office) Have a seat wherever you’re most comfortable.
Robert: Thank you. (Sits down, looks a bit nervous)
Dr. Santos: So, I know first sessions can feel a bit awkward or strange — you’re talking to someone you’ve just met about personal things. That’s completely normal. We’ll take things at your pace today.
Robert: Okay, that’s good to hear. I am feeling a bit nervous, actually.
Dr. Santos: That’s very understandable. Before we get into what brings you here today, I need to go over some important information about how therapy works and confidentiality. It might feel a bit formal at first, but it’s important that you know what to expect. Does that sound okay?
Robert: Yes, sure.
Part 2: Explaining Confidentiality
Dr. Santos: Great. So, first of all, everything we discuss in our sessions together is confidential. That means I don’t share what you tell me with anyone else without your written permission. This confidentiality is really important because I want you to feel safe talking openly about whatever is on your mind.
Robert: Okay, that’s clear to me.
Dr. Santos: However, there are a few limits to confidentiality that I’m legally required to tell you about. If I believe you’re at risk of harming yourself or someone else, or if there’s suspected abuse of a child or vulnerable adult, then I would need to take action to ensure safety. Also, if a court orders me to release records, I will have to comply. But in all of these situations, I would discuss it with you first whenever possible. Do you have any questions about confidentiality?
Robert: No, I think I understand. Those exceptions make sense.
Dr. Santos: Good. And just so you know, you can ask questions at any time — either today or in future sessions. This is your time, and I want you to feel comfortable.
Part 3: Discussing the Therapy Process
Dr. Santos: So, let me tell you a bit about how we typically work. Sessions last 50 minutes, and most people find that meeting weekly works well, at least initially. We’ll work together to identify your goals and figure out the best approach to help you. My style is collaborative — that means we’re working as a team. You’re the expert on your own life, and I’m here to provide support, tools, and a different perspective.
Robert: That sounds good. I was worried you might just tell me what to do.
Dr. Santos: (Smiles) No, therapy is really a collaborative process. I’ll offer suggestions and we’ll explore different strategies, but ultimately, you’re making the decisions about your life. My role is to support you, ask questions that might help you see things differently, and provide evidence-based techniques that might be helpful.
Robert: Okay, I like that approach.
Dr. Santos: I’m glad. Now, I do want to mention that therapy can sometimes be uncomfortable. When we talk about difficult experiences or emotions, it can bring up challenging feelings. That’s actually a normal part of the process, and it often means we’re working on something important. But I’ll always check in with you about how you’re doing, and we can adjust our pace as needed.
Part 4: Exploring the Client’s Concerns
Dr. Santos: So, Robert, tell me — what brings you to therapy?
Robert: Well, I’ve been struggling with anxiety for a while now, maybe about six months. It’s been getting worse recently, and it’s starting to affect my work.
Dr. Santos: I appreciate you sharing that. When you say “anxiety”, what does that look like for you? What are you experiencing?
Robert: It’s mostly worry. I worry about everything — work performance, what people think of me, whether I’m making mistakes. And physically, I feel tense a lot. My heart races sometimes, especially at meetings.
Dr. Santos: That sounds really challenging. It takes a lot of energy to carry that constant worry around. You mentioned it’s affecting your work. Can you tell me more about that?
Robert: Yeah, I’m having trouble concentrating. I keep second-guessing my decisions. I even avoided a presentation last week because I was so anxious about it.
Dr. Santos: I hear you. It sounds like the anxiety is limiting what you feel able to do. That must be frustrating.
Robert: It really is. I used to be more confident.
Part 5: Beginning Goal-Setting
Dr. Santos: Robert, if our work together is successful, what would be different for you? What change would you like to see?
Robert: I’d like to feel calmer, more in control. And I want to be able to do my job without this constant worry hanging over me.
Dr. Santos: Those are great goals. Feeling calmer, having more control, and being able to engage fully with your work. We can definitely work on those things together. In our future sessions, we’ll explore where this anxiety comes from and develop practical strategies to help you manage it.
Robert: That would be really helpful.
Dr. Santos: (Glancing at clock) We’re coming toward the end of our time today. Before we finish, I want to check in — how are you feeling about our conversation today?
Robert: I feel good, actually. I was nervous coming in, but I feel like you understand what I’m going through.
Dr. Santos: I’m so glad to hear that. It takes courage to take this step and come to therapy, and I want you to know that I’m committed to supporting you through this process. Let’s schedule our next session for the same time next week. Does that work for you?
Robert: Yes, that works.
Dr. Santos: Perfect. And Robert, if anything urgent comes up between now and then, you can call the office. But otherwise, I’ll see you next week. Take care.
Robert: Thank you, Dr. Santos. See you next week.
TASK 1: Comprehension and Analysis
Answer these questions about the dialogue:
1. How does Dr. Santos make Robert feel comfortable at the beginning?
2. What does Dr. Santos explain about confidentiality?
3. What are the limits to confidentiality that she mentions?
4. How does Dr. Santos describe the therapy process?
5. What type of questions does Dr. Santos use to explore Robert’s concerns?
6. What are Robert’s main goals for therapy?
7. How does Dr. Santos show empathy during the conversation?
8. What does Dr. Santos do at the end of the session?
TASK 2: Identifying Communication Techniques
Find examples in the dialogue where Dr. Santos uses these rapport-building techniques:
1. Normalizing the client’s experience: _______
2. Asking open-ended questions: _______
3. Reflecting/validating feelings: _______
4. Explaining the collaborative nature of therapy: _______
5. Checking in on the client’s comfort: _______
6. Summarizing what the client said: _______
7. Acknowledging the client’s courage: _______
TASK 3: Role Play Practice
Work in pairs. Student A is the therapist, Student B is the client.
Scenario 1: A new client’s first session. The client is feeling depressed and withdrawn. Practice:
• Greeting and creating comfort
• Explaining confidentiality
• Using open-ended questions
• Building rapport
Scenario 2: A client who is anxious about confidentiality. Practice:
• Addressing their concerns
• Explaining limits clearly
• Checking for understanding
Scenario 3: A first session with a client who has been in therapy before (but with a different therapist). Practice:
• Asking about previous experience
• Discussing expectations
• Collaborative goal-setting
ㅤ
TASK 4: Discussion Questions
Discuss with a partner or in small groups:
1. Why do you think the therapeutic alliance is so important?
2. What might happen if a therapist doesn’t explain confidentiality clearly?
3. How can a therapist balance being warm and friendly while maintaining professional boundaries?
4. What cultural differences might affect how rapport is built in the first session?
5. Why is it important to give clients choice and control from the first meeting?
6. How would you feel as a client in your first therapy session?
PROFESSIONAL PRACTICE:
Introducing the Therapeutic Framework and Informed Consent
Understanding how to explain the therapeutic framework and obtain informed consent is a critical professional skill for all mental health practitioners.
Key Components to Cover in a First Session
1. Welcome and Orientation
Create a warm, welcoming environment from the moment of first contact. Your goal is to help the client feel safe and comfortable enough to share personal information.
Sample language:
• “Welcome. I’m glad you’re here. Please, have a seat wherever you feel comfortable”.
• “I know it can feel a bit uncomfortable talking to someone new about personal matters. That’s completely normal, and we’ll take things at your pace”.
• “Before we begin, do you have any immediate questions or concerns?”
2. Explaining Confidentiality
Sample language:
• “Everything we discuss in our sessions is confidential. This means I don’t share what you tell me with anyone without your written permission”.
• “Confidentiality is essential because I want you to feel safe talking openly about whatever is on your mind”.
• “However, there are some important limits I need to tell you about…”
Explaining the limits:
• “If I believe you are at serious risk of harming yourself, I will need to take steps to ensure your safety”.
• “If I believe you are at risk of harming someone else, I have a duty to warn”.
• “If I suspect abuse or neglect of a child, elderly person, or dependent adult, I’m legally required to report it”.
• “If a court orders me to release records through a subpoena, I will have to comply”.
• “In all of these situations, I would discuss it with you whenever possible”.
Always ask: “Do you have any questions about confidentiality?”
3. Explaining the Therapy Process
Sample language:
• “Our sessions will last 50 minutes, and most people find weekly sessions work well at first”.
• “Therapy is a collaborative process. We’ll work together to identify your goals and figure out the best approach”.
• “My role is to listen, ask questions, offer different perspectives, and teach you tools and strategies that might help”.
• “Your role is to be as open and honest as you feel comfortable being, and to let me know if something isn’t working for you”.
• “I should mention that therapy can sometimes be uncomfortable. When we discuss difficult experiences or emotions, it can bring up challenging feelings. This is often a normal part of the process”.
4. Discussing Boundaries
Sample language:
• “Our sessions will take place here at this office, at the same time each week if that works for you”.
• “If you need to contact me between sessions, you can call the office and leave a message. I typically return calls within 24 hours”.
• “For emergencies, I’ll give you information about who to contact”.
• “Our relationship is a professional one, which means we won’t have contact outside of these sessions beyond what’s necessary for your treatment”.
5. Collaborative Goal-Setting
Sample language:
• “What would you like to achieve through our work together?
• “If therapy is successful, what will be different in your life?”
• “What would you like to focus on first?”
• “These goals will help guide our work and help us track your progress”.
6. Checking for Understanding and Comfort
Throughout the session:
• “Does that make sense?”
• “Do you have any questions about what I’ve explained?”
• “How are you feeling about what we’ve discussed so far?”
• “Is there anything you’d like me to clarify?”
7. Closing the Session
Sample language:
• “We’re coming to the end of our time today. Let me summarize what we’ve discussed…”
• “I want to acknowledge that it takes courage to come to therapy, and I appreciate you sharing with me today”.
• “How are you feeling about our conversation today?”
• “Let’s schedule our next session. Does the same time next week work for you?”
• “If anything urgent comes up before then, please call the office”.
Practice Exercises
ㅤ
Exercise 1: Explaining Confidentiality
Write a short explanation of confidentiality and its limits that you would give to a new client. Include:
• The general principle of confidentiality
• Why it’s important
• The specific limits
• An invitation for questions
Exercise 2: Responding to Client Questions
How would you respond to these client questions?
1. “Will you tell my family what we talk about?”
2. “What happens if I tell you I’m thinking about hurting myself?”
3. “Can we be friends on social media?”
4. “Can I text you between sessions?”
5. “How long will I need to be in therapy?”
6. “What if therapy doesn’t help?”
ㅤ
Exercise 3: Building Your Own Script
Create your own introduction for the first session. Include:
• Greeting and creating comfort
• Brief overview of what will happen in the session
• Explanation of confidentiality
• Description of the therapy process
• Invitation to share what brings them to therapy
Practice your script with a partner, then get feedback.
Exercise 4: Role Play
In pairs, practice a first session. One person is the therapist, one is the client.
Therapist tasks:
• Create a welcoming environment
• Explain informed consent and confidentiality
• Use open-ended questions
• Practise active listening
• Build rapport
• Collaboratively set initial goals
• Close the session appropriately
Client tasks:
• Be yourself, or role-play a specific scenario
• Ask questions about confidentiality or the process
• Share a concern (real or imagined)
• Give feedback to the therapist afterward
After 15–20 minutes, switch roles.
Vocabulary and Collocations for Unit 2
rapport — раппорт, контакт
therapeutic alliance — терапевтический альянс
confidentiality — конфиденциальность
boundaries — границы
informed consent — информированное согласие
safe space — безопасное пространство
initial therapy session — первая терапевтическая сессия
professional encounter — профессиональная встреча
make an appointment — записаться на прием
feeling anxious — чувствующий тревогу/испытывающий чувство тревоги
uncertain — неуверенный
vulnerable — уязвимый
foundation of trust — основа доверия
collaborative relationship — совместные отношения
first impression — первое впечатление
make eye contact — устанавливать зрительный контакт
warm greeting — теплое приветствие
speak freely — говорить свободно
opening conversation — вступительная беседа
at your pace — в вашем темпе
legal formality — юридическая формальность
ethical cornerstone — краеугольный камень этики
empower clients — наделять клиентов полномочиями
establish transparency — установить прозрачность
private information — частная информация
risk of harming — риск причинения вреда
suspected abuse — подозреваемое насилие
therapeutic boundaries — терапевтические границы
professional limits — профессиональные ограничения
session structure — структура сессии
contact between sessions — контакт между сессиями
social media policies — правила/политика социальных сетей
physical boundaries — физические границы
role clarity — ясность ролей
build trust — выстраивать доверие
build rapport — выстраивать раппорт
open-ended question — открытый вопрос
active listening — активное слушание
empathy — эмпатия
unconditional positive regard — безусловное позитивное принятие
validation — валидация
appropriate self-disclosure — уместное самораскрытие
therapeutic relationship — терапевтические отношения
positive therapy outcomes — позитивные результаты терапии
collaborative goal-setting — совместная постановка целей
track progress — отслеживать прогресс
client — клиент
collaborative — совместный
establish boundaries — устанавливать границы
verbal consent — устное согласие
confide — доверять
confidential — конфиденциальный
comfortable — удобный, комфортный
collaborate — сотрудничать
collaboration — сотрудничество
empower — наделять полномочиями
empowerment — наделение полномочиями
empowered — наделенный полномочиями
sympathy — сочувствие
borders — границы (географические)
knowledgeable — осведомленный
collective goals — совместные/коллективные/общие цели
UNIT 3.
INITIAL ASSESSMENT
LEAD-IN:
Information Gathering and Sensitive Questioning Skills
Activity 1: Role-play everyday information gathering
Work in pairs. Take turns asking personal questions in these everyday situations:
• Meeting a new neighbour who has just moved in
• Interviewing someone for a shared apartment
• Getting to know a colleague at a new job
Discuss: What questions did you ask? Which questions felt comfortable? Which felt too personal?
Activity 2: What information matters?
Look at the list below. When meeting a client for the first time, which information is most important to gather? Rank these from 1 (most important) to 10 (least important):
• Current problem/reason for seeking help
• Family background
• Medical history
• Work/education history
• Past mental health treatment
• Current medications
• Social support system
• Childhood experiences
• Current living situation
• Hobbies and interests
Compare your rankings with a partner. Explain your choices.
Activity 3: Sensitive vs. direct questioning quiz
Which question is more appropriate for an initial assessment? Discuss why:
1. a) Have you ever tried to kill yourself?
b) Have you ever had thoughts of harming yourself or ending your life?
2. a) Tell me about your drinking habits.
b) Do you drink alcohol?
3. a) Why did you come here today?
b) What brings you here today?
4. a) Are you depressed?
b) How would you describe your mood lately?
5. a) Do you have problems with your family?
b) Tell me about your relationships with family members.
Note: Most questions require question marks. But in clinical practice open-ended alternatives using imperatives like “Tell me about…” or “Describe…” are also acceptable as questions, though they are technically requests rather than questions.
Key vocabulary for this unit:
ㅤ
Match the words with their definitions:
1. Presenting problem
2. Intake interview
3. Chief complaint
4. Psychosocial history
5. Risk assessment
6. Mental status examination
7. Rapport
8. Confidentiality
ㅤ
a) The main issue that brings a client to seek help
b) First session designed to gather comprehensive background information
c) Evaluation of potential danger to self or others
d) Systematic observation of a client’s psychological functioning
e) Information about personal, family, social, and cultural background
f) A trusting, comfortable connection between therapist and client
g) The primary symptom or concern in the client’s own words
h) The principle that client information remains private
READING:
Understanding the Presenting Problem: Initial Assessment
Pre-reading task
Before you read, discuss:
1. What do you think happens in the first session with a client?
2. What information should a psychologist gather during an intake interview?
3. Why is it important to understand the “presenting problem”?
4. What is a mental status examination?
ㅤ
Understanding the Presenting Problem: Initial Assessment
When a client first contacts a psychologist, one of the most important tasks is conducting a comprehensive initial assessment or intake interview. This first session sets the foundation for the entire therapeutic relationship and treatment process. The psychologist gathers essential information, establishes rapport, and begins to understand the client’s difficulties within the context of their life.
The Purpose of Initial Assessment
The initial assessment serves multiple purposes. First, it allows the psychologist to understand why the client is seeking help — what professionals call the presenting problem or chief complaint. This is the primary issue or concern that brings the client to therapy, described in the client’s own words. Second, the assessment provides comprehensive background information about the client’s personal history, current life situation, and past experiences with mental health issues. Third, it helps the psychologist determine whether they can help the client or whether a referral to another professional would be more appropriate.
The initial assessment is also the beginning of the therapeutic relationship. During this first session, the psychologist works to establish rapport — a trusting, comfortable connection with the client. Without rapport, clients may not feel safe enough to share sensitive information or engage fully in the therapeutic process. The psychologist demonstrates empathy, active listening, and respect while maintaining professional boundaries and explaining important concepts like confidentiality.
Gathering the Presenting Problem
The assessment typically begins with an open-ended question designed to let the client tell their story in their own way. Common opening questions include: “What brings you here today?” or “What’s been happening that led you to seek help now?” These questions invite narrative responses rather than simple yes/no answers.
As the client describes their presenting problem, the psychologist listens carefully and asks follow-up questions to clarify the nature of the difficulty. Important aspects to explore include:
• Onset: When did the problem begin? Was there a specific event or trigger?
• Duration: How long has the problem been present?
• Frequency: How often does the problem occur?
• Severity: How much does the problem interfere with daily functioning?
• Previous attempts: What has the client tried to address the problem? What worked or didn’t work?
• Client’s understanding: What does the client think is causing the problem? What are their expectations for treatment?
For example, a client might say: “I’ve been feeling really anxious lately”. The psychologist would then explore: When did the anxiety start? What situations trigger it? How does it affect your daily life? What have you tried to manage it? This detailed exploration helps the psychologist understand not just the symptom, but the context surrounding it.
Taking the Psychosocial History
After exploring the presenting problem, the psychologist gathers information about the client’s psychosocial history — their personal, family, social, educational, occupational, and medical background. This comprehensive history helps the psychologist understand the client as a whole person and identify factors that may contribute to current difficulties.
Key areas of psychosocial history include:
Developmental and family history: information about childhood, family structure, relationships with parents and siblings, significant early experiences, and any history of abuse or trauma.
Educational and occupational history: school performance, level of education, current employment status, job satisfaction, and any work-related stress.
Relationship and social history: current and past romantic relationships, friendships, social support network, and quality of interpersonal relationships.
Medical history: physical health conditions, current medications, past surgeries or hospitalizations, and any chronic illnesses.
Past psychiatric history: previous mental health diagnoses, past therapy or counselling experiences, psychiatric hospitalizations, and any history of psychotropic medication use.
Substance use: current and past use of alcohol, tobacco, and other substances.
The psychologist uses a combination of open-ended and closed-ended questions to gather this information efficiently while still allowing the client to share their story. For example, a closed-ended question like “Are you currently employed?” establishes a fact, while an open-ended follow-up like “Tell me about your work situation invites the client to provide context and detail”.
Conducting a Mental Status Examination
An essential component of the initial assessment is the mental status examination (MSE) — a systematic observation and description of the client’s current psychological functioning. While some aspects of the MSE are observed naturally during the interview, psychologists may also ask specific questions to assess certain domains.
The MSE typically evaluates the following areas:
Appearance and behaviour: the psychologist observes how the client looks (grooming, clothing, hygiene) and behaves (eye contact, posture, motor activity, unusual movements).
Speech: rate, volume, tone, and any abnormalities in speech patterns.
Mood and affect: mood is the client’s subjective emotional state (how they say they feel), while affect is the observable emotional expression. Psychologists assess whether affect is appropriate to the content being discussed, its range (restricted, normal, or labile), and its intensity.
Thought process: how the client thinks — whether their thoughts are logical, organized, and goal-directed, or whether there are signs of disorganization, tangentiality, or circumstantiality.
Thought content: what the client thinks about — including any delusions, obsessions, preoccupations, or suicidal/homicidal ideation.
Perception: whether the client experiences hallucinations (seeing or hearing things that aren’t there) or other perceptual disturbances.
Cognition: assessment of orientation (awareness of time, place, and person), attention, concentration, memory, and general intellectual functioning.
Insight and judgment: the client’s awareness of their condition and their ability to make sound decisions.
The MSE provides a “snapshot” of the client’s mental state at the time of the assessment and helps identify symptoms that may indicate specific mental health conditions.
Risk Assessment
A critical component of any initial assessment is evaluating risk — particularly the risk of self-harm, suicide, or harm to others. Psychologists must directly but sensitively ask about these concerns. Contrary to common fears, asking about suicidal thoughts does not increase the risk; instead, it demonstrates care and creates an opportunity for the client to discuss difficult feelings.
Risk assessment questions might include: Have you had any thoughts of harming yourself? Have you had thoughts of ending your life? Do you have a specific plan? If a client endorses suicidal thoughts, the psychologist assesses the frequency, intensity, duration, and whether the person has means and intent to carry out a plan. Protective factors, such as reasons for living, social support, and future orientation, are also explored.
Formulating and Planning
At the conclusion of the initial assessment, the psychologist integrates all the information gathered to develop a preliminary understanding of the client’s difficulties. Many psychologists use a formulation framework called the Four Ps:
• Predisposing factors: background factors that make the person vulnerable (e.g., family history of mental illness, early trauma)
• Precipitating factors: recent events or stressors that triggered the current problem (e.g., job loss, relationship breakup)
• Perpetuating factors: factors that maintain or worsen the problem (e.g., poor coping strategies, lack of social support, avoidance behaviours)
• Protective factors: strengths and resources that can aid recovery (e.g., supportive relationships, resilience, motivation for change)
This formulation guides treatment planning and helps the psychologist and client work collaboratively toward meaningful goals.
Comprehension Questions
1. What is the purpose of the initial assessment?
2. What is the difference between “presenting problem” and “chief complaint”?
3. Why is rapport important in the first session?
4. What are the five key aspects to explore when gathering information about the presenting problem?
5. What types of information are included in a psychosocial history?
6. What is the difference between mood and affect in the MSE?
7. Why do psychologists ask about suicidal thoughts during initial assessment?
8. What are the “Four Ps” in formulation?
9. According to the text, what is the difference between open-ended and closed-ended questions?
10. What areas does a mental status examination cover?
VOCABULARY:
Assessment Terminology and Mental Status Examination
A. Find words in the text that match these definitions:
1. The main problem that brings a client to therapy (paragraph 2): _______
2. A relationship based on empathy and respect between therapist and client (paragraph 3): _______
3. The beginning or start of a problem (paragraph 4): _______
4. How often something happens (paragraph 4): _______
5. Information about personal, family, and social background (paragraph 5): _______
6. A client’s subjective description of their emotional state (paragraph 8): _______
7. The observable emotional expression (paragraph 8): _______
8. Awareness of one’s condition (paragraph 8): _______
9. False beliefs not based on reality (paragraph 8): _______
10. Factors that maintain or worsen a problem (paragraph 10): _______
B. Complete the collocations from the text:
1. initial _______
2. intake _______
3. presenting _______
4. mental _______ examination
5. psychosocial _______
6. risk _______
7. _______ rapport
8. _______ confidentiality
9. treatment _______
10. protective _______
11. coping _______
12. therapeutic _______
13. follow-up _______
14. open-ended _______
15. suicidal _______
ㅤ
C. Word families
Complete the table:
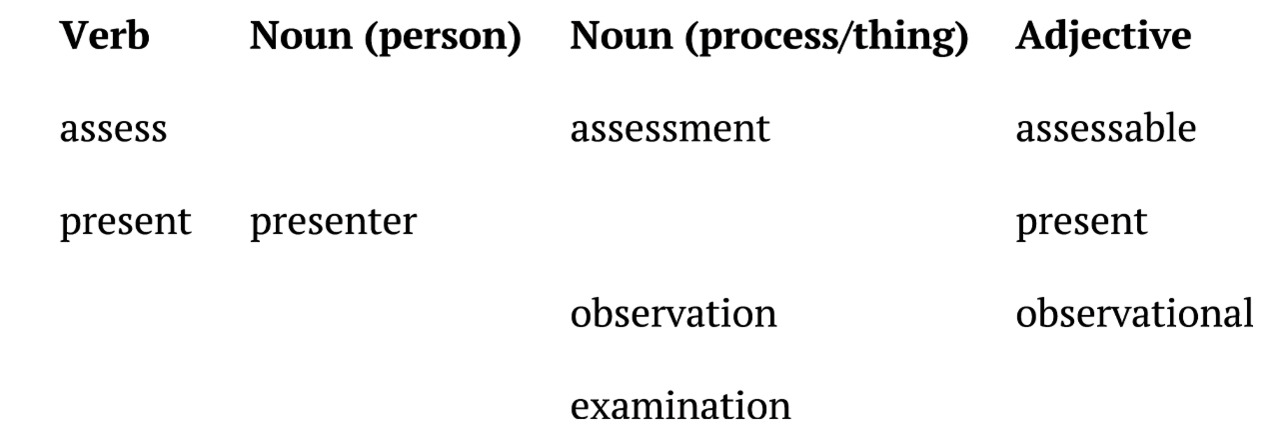
D. Match the MSE terms with descriptions:
1. Affect
2. Thought process
3. Orientation
4. Delusion
5. Hallucination
6. Insight
7. Labile affect
8. Tangentiality
ㅤ
a) Observable emotional expression
b) False belief firmly held despite evidence
c) Awareness of one’s condition
d) Rapidly changing emotions
e) Awareness of time, place, and person
f) Perceiving something that isn’t there
g) How thoughts are organized and connected
h) Going off-topic when speaking
ㅤ
Discussion Questions
1. In your country, how is the first psychology session typically structured?
2. What cultural factors might influence how clients describe their presenting problems?
3. How can psychologists establish rapport with clients who are reluctant to share personal information?
4. Do you think it’s appropriate to ask about suicidal thoughts in every initial assessment? Why or why not?
5. What challenges might arise when gathering psychosocial history from clients of different cultural backgrounds?
6. How would you feel about asking personal questions during an intake interview?
7. Which area of the mental status examination do you think is most important? Why?
8. How might the Four Ps formulation help in understanding a client’s difficulties?
GRAMMAR FOCUS:
Past Simple and Past Continuous for Client History / Question Forms
A. Past Simple for Completed Events in Client’s History
We use Past Simple to ask about and describe completed events, experiences, and situations in a client’s past:
Form:
• Affirmative: Subject + verb + -ed (regular) / irregular form
• Negative: Subject + didn’t + main verb
• Questions: Did + subject + main verb?
• Wh-questions: When/Where/Why + did + subject + main verb?
Examples from Assessment:
✓ When did your symptoms first start?
✓ The client experienced anxiety attacks for the first time in 2020.
✓ She didn’t seek help until last month.
✓ Did you have any support during that time?
✓ How did you cope with the loss?
✓ He received therapy three years ago.
Time expressions with Past Simple:
• yesterday, last week/month/year, ago, in 2020, when I was…, at that time
Exercise 1: Complete the intake questions
Use the correct form of the verb in brackets:
1. When _______ (do) you first notice these symptoms?
2. How long _______ (do) the symptoms last?
3. _______ (you/try) any strategies to manage the problem?
4. What _______ (happen) after you lost your job?
5. How _______ (you/feel) when that happened?
6. The client _______ (not/experience) depression until recently.
7. He _______ (have) several panic attacks last month.
B. Past Continuous for Background and Context
We use Past Continuous to describe ongoing situations or actions in the past that provide context for events:
Form:
• Affirmative: Subject + was/were + main verb + -ing
• Negative: Subject + wasn’t/weren’t + main verb + -ing
• Questions: Was/Were + subject + main verb + -ing?
Examples from Assessment:
✓ What were you doing when the panic attack started?
✓ She wasn’t sleeping well during that period.
✓ Were you experiencing any stress at work?
✓ He was going through a difficult divorce when the symptoms began.
Using Past Simple and Past Continuous together:
We often use both tenses to show how events relate to each other:
✓ I was driving to work when I had my first panic attack. (Past Continuous for background + Past Simple for main event)
✓ While she was dealing with her mother’s illness, she started having sleep problems. (Past Continuous for context + Past Simple for specific problem)
Exercise 2: Past Simple or Past Continuous?
Choose the correct form:
1. When (did the symptoms start / were the symptoms starting)?
2. What (did you do / were you doing) when you felt the anxiety?
3. She (didn’t cope / wasn’t coping) well with the stress at that time.
4. While he (studied / was studying) for exams, he (developed / was developing) insomnia.
5. (Did you experience / Were you experiencing) any major life changes before this?
6. The problems (began / were beginning) when I (worked / was working) at my previous job.
7. (Did she take / Was she taking) medication when she (came / was coming) to see you?
8. They (had / were having) financial difficulties when their relationship (broke down / was breaking down).
C. Question Forms: Open-ended vs. Closed-ended
Closed-ended questions require yes/no or brief factual answers:
✓ Do you have any children?
✓ Are you currently employed?
✓ Have you been hospitalized before?
✓ Did you finish high school?
Open-ended questions encourage detailed, narrative responses:
✓ What brings you here today?
✓ How would you describe your relationship with your family?
✓ What happened when you lost your job?
✓ How have you been coping with these feelings?
Wh-questions for assessment:
• What = specific information about problems, situations, thoughts
• When = timeline, onset, duration
• Where = location, context, settings
• Who = people involved, support system
• How = manner, coping strategies, severity
• Why = reasons, motivation (use carefully — can sound judgmental)
Exercise 3: Rewrite as open-ended questions
1. Are you stressed at work? → _______
2. Do you have a good relationship with your parents? → _______
3. Did something bad happen in your childhood? → _______
4. Are you sleeping well? → _______
5. Do you drink alcohol? → _______
6. Are you worried about anything? → _______
Exercise 4: Correct the mistakes
Find and correct the mistakes in these assessment questions:
1. When was happening the problem?
2. What you were doing when you felt anxious?
3. Did you was experiencing stress at that time?
4. She wasn’t cope well with the situation.
5. Were you felt depressed last year?
6. What did happened after you lose your job?
7. He didn’t was sleeping well during that period.
8. While I working, I had a panic attack.
COMMUNICATION:
Conducting an Initial Assessment: Sample Interview Excerpts
Excerpt 1: Opening and Presenting Problem
Psychologist: Good morning, Maria. Thank you for coming in today. Before we begin, I’d like to explain that everything we discuss is confidential unless there’s a risk of harm to yourself or others. Do you have any questions about that?
Maria: No, that’s clear. Thank you.
Psychologist: Great. So, what brings you here today?
Maria: Well, I’ve been feeling really anxious for the past few months. It’s getting worse, and I’m having trouble concentrating at work.
Psychologist: I see. When did you first notice these anxiety symptoms?
Maria: It started around March, I think. I was working on a big project at work, and I began having trouble sleeping.
Psychologist: And you mentioned it’s been getting worse. What’s been happening recently?
Maria: Last week I had what I think was a panic attack. My heart was racing, I couldn’t breathe properly, and I thought I was having a heart attack. It was terrifying.
Psychologist: That sounds very frightening. Where were you when this happened?
Maria: I was at work, in the middle of a meeting. I had to leave the room.
Psychologist: What did you do after you left the meeting?
Maria: I went to the bathroom and tried to calm down. A colleague found me and sat with me until I felt better. That’s actually when she suggested I should talk to someone.
Psychologist: It’s good that you had support. Before this panic attack, had you experienced anything like that before?
Maria: Not to that extent, no. But I’ve been feeling on edge for months now.
Excerpt 2: Psychosocial History
Psychologist: Maria, I’d like to understand more about your background. Tell me about your family.
Maria: Well, I’m 32 years old. I live alone, but my parents and younger brother live in the same city. We’re quite close.
Psychologist: How would you describe your relationship with your family?
Maria: It’s good, mostly. My parents are supportive, but they can be rather demanding. They have high expectations, especially about my career.
Psychologist: And you mentioned you have a younger brother. How is your relationship with him?
Maria: We get along well. He’s five years younger than me, so we weren’t that close growing up, but now we talk regularly.
Psychologist: What about your social life outside of family? Tell me about your friendships.
Maria: I have a few close friends from university. We try to meet up regularly, but with work being so busy, it’s been difficult lately. I’ve actually been avoiding social activities because I feel so anxious.
Psychologist: You mentioned work several times. Tell me about your job.
Maria: I’m a marketing manager at a tech company. I’ve been there for four years. I used to love the job, but lately the pressure has been intense. We had layoffs last year, so those of us who remained have much heavier workloads.
Psychologist: That sounds stressful. Were you working there when the anxiety started?
Maria: Yes, the anxiety definitely got worse after the layoffs. I kept worrying that I might be next.
Excerpt 3: Past Psychiatric History and Substance Use
Psychologist: Have you ever experienced symptoms like this before, Maria?
Maria: Not really. I mean, I’ve always been a bit of a worrier, but nothing like this.
Psychologist: Have you ever sought help for mental health concerns before?
Maria: No, this is my first time seeing a psychologist. I always thought I could handle things on my own.
Psychologist: Have you ever been prescribed medication for anxiety or any other mental health condition?
Maria: No, never.
Psychologist: Is there any history of mental health issues in your family?
Maria: My mother has always been anxious too, but she’s never gotten treatment. She just says it’s “her personality.”
Psychologist: I see. Now I need to ask you some questions about substance use. Do you drink alcohol?
Maria: Yes, socially. Maybe a glass of wine with dinner once or twice a week.
Psychologist: Has your alcohol use changed recently?
Maria: Actually, yes. I’ve been drinking more in the evenings to help me relax. Maybe three or four glasses a few times a week.
Psychologist: And do you use any other substances — tobacco, cannabis, or anything else?
Maria: No, just alcohol.
Excerpt 4: Risk Assessment
Psychologist: Maria, I need to ask you some important questions about how you’ve been coping. Have you had any thoughts of harming yourself?
Maria: [pause] Sometimes I feel so overwhelmed that I just wish I could disappear. But I haven’t actually thought about hurting myself, if that’s what you mean.
Psychologist: Thank you for being honest. When you say you wish you could disappear, what do you mean by that?
Maria: I just mean I want a break from all the pressure and anxiety. I want to feel normal again.
Psychologist: That makes sense. Have you had any specific thoughts about ending your life?
Maria: No, nothing like that. I would never do that to my family.
Psychologist: That’s important to know. What helps you get through difficult moments?
Maria: Talking to my best friend helps. And sometimes I go for walks to clear my head.
Psychologist: It sounds like you’ve found some helpful strategies. I’m glad you have some support and coping methods in place.
TASK 1: True / False / Not Mentioned
Read the statements below about Maria’s interview. Decide if each statement is:
• TRUE (T) — the statement agrees with the information
• FALSE (F) — the statement contradicts the information
• NOT MENTIONED (N/M) — the information is not given
Statements:
1. Maria’s anxiety symptoms began in March.
2. Maria had her first panic attack at home.
3. Maria has seen a psychologist before.
4. Maria’s mother has been treated for anxiety.
5. Maria lives with her parents.
6. Maria’s workplace had layoffs last year.
7. Maria has been avoiding social activities recently.
8. Maria drinks alcohol every day.
9. Maria has suicidal thoughts.
10. Maria finds that talking to her best friend helps her cope.
TASK 2: Comprehension and Note-Taking
Read the interview excerpts carefully. Complete Maria’s intake form:
Client Intake Form
Name: Maria
Age: _______
Presenting Problem: _______
Onset: _______
Recent Crisis Event: _______
Living Situation: _______
Family: _______
Occupation: _______
Work-related Stressors: _______
Past Mental Health Treatment: _______
Family Mental Health History: _______
Substance Use: _______
Current Coping Strategies: _______
Suicidal Ideation: _______
Protective Factors: _______
TASK 3: Analyzing Question Types
Review the interview excerpts. Identify five open-ended questions and five closed-ended questions the psychologist asked. Discuss why each type was used at that moment.
Open-ended questions:
1. ________________________________________
2. ________________________________________
3. ________________________________________
4. ________________________________________
5. ________________________________________
Closed-ended questions:
1. ________________________________________
2. ________________________________________
3. ________________________________________
4. ________________________________________
5. ________________________________________
ㅤ
TASK 4: Role-Play Practice
Work in pairs. Student A is the psychologist; Student B is the client.
Scenario 1: Client presenting with sleep problems and work stress
Scenario 2: Client presenting with relationship difficulties and low mood
Scenario 3: Client presenting with social anxiety and isolation
Psychologist tasks:
• Open the session and explain confidentiality
• Ask about the presenting problem using open-ended questions
• Explore onset, duration, frequency, and severity
• Gather brief psychosocial history
• Ask appropriate risk assessment questions
Client tasks:
• Create a brief background story for your character
• Respond naturally to questions
• Provide enough detail but also some ambiguity that requires follow-up questions
After the role-play, switch roles and try a different scenario.
PROFESSIONAL PRACTICE:
Structuring an Initial Assessment Session
Sample Assessment Structure
A typical initial assessment session (usually 60—90 minutes) follows this general structure:
1. Introduction and Informed Consent (5–10 minutes)
• Introduce yourself and explain your role
• Explain confidentiality and its limits
• Discuss the structure and purpose of the session
• Answer any questions the client has
• Establish initial rapport
2. Presenting Problem (15–20 minutes)
• Use open-ended questions to understand why the client is seeking help
• Explore onset, duration, frequency, severity
• Identify triggers and patterns
• Understand the client’s perspective on the problem
• Explore previous attempts to address the issue
3. Psychosocial History (20—30 minutes)
• Developmental and family background
• Educational and occupational history
• Relationship and social history
• Medical history
• Past psychiatric history
• Substance use
4. Mental Status Examination (Ongoing throughout session)
• Observe appearance, behaviour, speech
• Assess mood and affect
• Note thought process and content
• Evaluate cognition, insight, and judgment
5. Risk Assessment (5–10 minutes)
• Assess suicidal ideation, intent, plan
• Assess risk of harm to others
• Identify protective factors
6. Summary and Next Steps (10 minutes)
• Summarize key information gathered
• Share preliminary impressions (when appropriate)
• Discuss treatment options and recommendations
• Schedule follow-up appointment
• Answer questions
Useful Phrases for Conducting Initial Assessment
Opening the Session:
• Thank you for coming in today.
• Before we begin, I’d like to explain how our session will work.
• Everything we discuss is confidential, with a few exceptions I’ll explain.
• Do you have any questions before we start?
• I’m here to listen and help you understand what’s been happening.
Exploring the Presenting Problem:
• What brings you here today?
• Tell me what’s been happening.
• When did you first notice this problem?
• How has this been affecting your daily life?
• What have you tried so far to address this?
• What made you decide to seek help now?
Gathering History:
• I’d like to learn more about your background.
• Tell me about your family.
• How would you describe your childhood?
• Walk me through your work history.
• Have you experienced mental health difficulties before?
• Is there any family history of mental health issues?
Asking Sensitive Questions:
• I need to ask some important questions that I ask everyone.
• These questions might feel uncomfortable, but they’re important for understanding your situation.
• Have you had any thoughts of harming yourself?
• Have you had thoughts of ending your life?
• Tell me about your alcohol use.
Showing Empathy and Building Rapport:
• That sounds very difficult.
• I can understand why that would be distressing.
• Thank you for sharing that with me.
• It takes courage to talk about these things.
• You’re not alone in experiencing this.
Clarifying and Following Up:
• Can you tell me more about that?
• What do you mean by…?
• Help me understand…
• Can you give me an example?
• How did that make you feel?
Transitioning Between Topics:
• Now I’d like to ask about a different area…
• Let’s talk about your work situation…
• I’d like to shift to discussing your family background…
• Moving on to another topic…
Closing the Session:
• We’re coming to the end of our time today.
• Let me summarize what I’ve heard…
• Based on what you’ve shared, I think we can work on…
• What questions do you have for me?
• Let’s schedule our next appointment.
Practice Exercises
Exercise 1: Create Your Opening Statement
Write your opening statement for an initial assessment session. Include:
• Introduction
• Explanation of confidentiality
• Structure of the session
• Invitation for questions
Exercise 2: Sequence the Assessment
Put these assessment components in the most logical order:
a) Risk assessment
b) Introduction and informed consent
c) Psychosocial history
d) Mental status examination
e) Presenting problem
f) Summary and treatment planning
Exercise 3: Open-Ended Question Practice
For each closed-ended question, write an open-ended alternative. There may be more than one variant:
1. Do you get along with your family?
2. Are you stressed?
3. Did you like school?
4. Do you have friends?
5. Are you taking any medications?
ㅤ
Exercise 4: Case Formulation — The Four Ps
Read this brief case and identify the Four Ps:
Tom is a 28-year-old software developer presenting with symptoms of depression. His father had depression, and Tom experienced bullying in high school. Three months ago, Tom’s long-term relationship ended, and shortly after, he began experiencing low mood, loss of interest, and sleep problems. Tom has been isolating himself from friends, spending most evenings alone, and has stopped exercising — activities that previously helped his mood. However, Tom has a supportive sister, a stable job, and expressed motivation to feel better.
Predisposing factors: _______
Precipitating factors: _______
Perpetuating factors: _______
Protective factors: _______
Exercise 5: Role-Play Assessment Practice
Work in groups of three: Psychologist, Client, Observer.
Instructions:
• Psychologist: Conduct a 10-minute initial assessment focusing on presenting problem
• Client: Use one of the scenarios provided or create your own
• Observer: Note down question types used, rapport-building techniques, and areas that could be explored further
After the role-play, the observer provides feedback.
Vocabulary and Collocations for Unit 3
presenting problem — предъявляемая проблема
intake interview — первичное интервью
chief complaint — основная жалоба
psychosocial history — психосоциальный анамнез
risk assessment — оценка риска
mental status examination (MSE) — исследование психического статуса
rapport — раппорт
confidentiality — конфиденциальность
initial assessment — первичная оценка
comprehensive background information — полная биография (клиента)
therapeutic relationship — терапевтические отношения
treatment process — процесс лечения
gather essential information — собирать существенную информацию
establish rapport — устанавливать раппорт
sensitive information — деликатная/конфиденциальная информация
engage fully — полностью включаться
maintain professional boundaries — поддерживать профессиональные границы
open-ended question — открытый вопрос
closed-ended question — закрытый вопрос
narrative responses — повествовательные ответы
follow-up questions — уточняющие вопросы
onset — начало
duration — продолжительность
frequency — частота
severity (of symptoms) — тяжесть (симптомов)
daily functioning — повседневное функционирование
previous attempts — предыдущие попытки
developmental history — история развития
family history — семейный анамнез
family structure — структура семьи
educational history — образовательный анамнез
occupational history — профессиональный анамнез
employment status — статус занятости
job satisfaction — удовлетворенность работой
work-related stress — связанный с работой стресс
relationship history — история отношений
social history — социальный анамнез
social support network — сеть социальной поддержки
interpersonal relationships — межличностные отношения
medical history — медицинский анамнез
current medications — принимаемые лекарства
chronic illnesses — хронические заболевания
past psychiatric history — предшествующий психиатрический анамнез
psychiatric hospitalizations — психиатрические госпитализации
psychotropic medication — психотропные препараты
substance use — употребление веществ
systematic observation — систематическое наблюдение
psychological functioning — психологическое функционирование
appearance and behaviour — внешний вид и поведение
eye contact — зрительный контакт
motor activity — моторная активность
speech patterns — речевые паттерны
mood — настроение
affect — аффект
emotional state — эмоциональное состояние
observable emotional expression — наблюдаемая эмоциональная экспрессия
labile affect — лабильный аффект
thought process — мыслительный процесс
thought content — содержание мыслей
delusions — бред
obsessions — обсессии/навязчивости
suicidal ideation — суицидальные мысли/идеи о самоубийстве
homicidal ideation — мысли об убийстве
perception — восприятие
hallucinations — галлюцинации
perceptual disturbances — нарушения восприятия
cognition — когниция
orientation — ориентация
attention — внимание
concentration — концентрация
memory — память
intellectual functioning — интеллектуальное функционирование
insight — инсайт/озарение
judgment — суждение
self-harm — самоповреждение
suicide — самоубийство
harm to others — вред другим
suicidal thoughts — суицидальные мысли
specific plan — конкретный план
protective factors — защитные факторы
reasons for living — причины жить
future orientation — ориентация на будущее
preliminary understanding — предварительное понимание
formulation framework — модель концептуализации случая
predisposing factors — предрасполагающие факторы
precipitating factors — провоцирующие факторы
perpetuating factors — поддерживающие факторы
early trauma — ранняя травма
recent events — недавние события
stressors — стрессоры
job loss — потеря работы
relationship breakup — разрыв отношений
poor coping strategies — плохие стратегии совладания
lack of social support — отсутствие социальной поддержки
avoidance behaviour — избегающее поведение
supportive relationships — поддерживающие отношения
resilience — устойчивость
motivation for change — мотивация к изменениям
treatment planning — планирование лечения
tangentiality — тангенциальность
circumstantiality — обстоятельность
vulnerable — уязвимый
informed consent — информированное согласие
transparency — прозрачность
active listening — активное слушание
empathy — эмпатия
unconditional positive regard — безусловное позитивное принятие
collaborative — совместный
coping strategies — стратегии совладания
UNIT 4.
TREATMENT PLANNING AND THERAPEUTIC SESSION
LEAD-IN:
Session Structure and Goal-Setting
Activity 1: Ordering therapy session stages
The stages of a typical therapy session are jumbled below. Put them in the correct order (1•6):
___ Working section (exploring issues, applying techniques)
___ Check-in (reviewing the week, current state)
___ Closing and homework assignment
___ Agenda setting (deciding session focus)
___ Summary of progress and key points
___ Bridge from previous session
Activity 2: Brainstorming — From the first session to termination
Work in small groups. You have 5 minutes to brainstorm and write down:
• Components of a first session (intake)
• Components of regular sessions
• Components of a final session (termination)
Share your ideas with the class.
Example components:
• First session: building rapport, gathering history, setting initial goals, explaining the therapeutic process…
• Regular sessions: check-in, agenda, interventions, homework review…
• Final session: reviewing progress, relapse prevention planning, saying goodbye…
Activity 3: Discussion questions
Discuss these questions with your partner:
1. Why is structure important in a therapy session?
2. How can a therapist and client determine if therapy is working?
3. What does “measuring progress” mean in psychotherapy?
4. Should every session follow the same structure, or should it be flexible?
5. When should therapy end? How do you know?
6. What is relapse prevention?
Key vocabulary for this unit:
Match the words with their definitions:
1. Check-in
2. Agenda setting
3. Treatment plan
4. SMART goals
5. Intervention
6. Termination
7. Relapse prevention
8. Homework
ㅤ
a) A structured document outlining objectives, methods, and expected outcomes of therapy
b) Brief opening discussion about the client’s current state and recent experiences
c) Goals that are Specific, Measurable, Achievable, Relevant, and Time-bound
d) Collaborative process of deciding what to focus on during the session
e) The planned ending of the therapeutic relationship
f) Therapeutic technique or strategy used to address client’s difficulties
g) Strategies to help clients maintain gains and avoid returning to problematic patterns
h) Tasks or practice activities assigned between sessions
READING:
Managing Sessions and Planning Treatment: From Structure to Goals
Pre-reading task
Before you read, discuss:
1. What do you think should happen at the beginning of every therapy session?
2. Why might clients need homework between sessions?
3. What makes a good therapy goal?
4. How should therapy end?
ㅤ
Managing Sessions and Planning Treatment: From Structure to Goals
Effective psychotherapy requires both skilled therapeutic intervention and careful planning. Whether working with clients experiencing depression, anxiety, trauma, or relationship difficulties, psychologists must structure their sessions thoughtfully and develop comprehensive treatment plans that guide the therapeutic process from the first meeting to successful termination.
The Therapeutic Frame and Session Structure
The concept of the therapeutic frame refers to the consistent boundaries and structure that provide safety and predictability in therapy. This includes the regular time and place of sessions, duration (typically 45–60 minutes), confidentiality agreements, and the overall format of each meeting. A consistent therapeutic frame helps clients feel secure and allows them to focus on their inner experience rather than worrying about unpredictable elements.
Each therapy session, whether it is the second meeting or the twentieth, generally follows a recognizable structure that includes several key components. This structure provides organization while remaining flexible enough to respond to clients’ immediate needs.
The session typically begins with a check-in, a brief opening where the therapist asks about the client’s current state and experiences since the last meeting. During check-in, clients might share how their week went, whether they experienced any significant events, or how they are feeling in the present moment. This helps the therapist assess the client’s immediate emotional state and determine if any crisis or urgent issue requires immediate attention. For example, a therapist might ask, “How have things been since we last met?” or “What’s been on your mind this week?”
Following the check-in comes agenda setting, a collaborative process where therapist and client decide together what to focus on during the session. The therapist might say, “What would be most helpful to work on today?” or “Let’s think about what we want to accomplish in our time together.” Agenda setting empowers clients by giving them voice in their treatment and ensures that sessions address their most pressing concerns. The agenda might include reviewing homework from the previous session, discussing a recent difficult situation, practicing a new skill, or exploring a longstanding pattern.
The working section forms the main body of the session, where the therapeutic work takes place. This is when a therapist and a client engage with the chosen agenda items using various therapeutic techniques and interventions. In CBT, this might involve identifying and challenging negative automatic thoughts. In psychodynamic therapy, it might mean exploring unconscious patterns or discussing transference. In humanistic therapy, the therapist might reflect the client’s feelings and help them explore their experience more deeply. The working section is flexible and responsive to what emerges during the conversation.
As the session approaches its end, the therapist initiates closing and summary. During this phase, the therapist and client review what was discussed, highlight key insights or progress, and ensure the client feels grounded before leaving. The therapist might ask, “What are you taking away from today’s session?” or “How are you feeling right now?” This is also the time for homework assignment — therapeutic tasks that help clients practice new skills or continue therapeutic work between sessions. Homework might include keeping a thought diary, practicing relaxation techniques, or trying new behaviour in a real-life situation.
Research shows that clients who complete homework assignments between sessions make faster progress and achieve better outcomes. Homework bridges the gap between the therapy room and real life, allowing clients to apply what they learn in session to their daily experiences.
Treatment Planning: Creating a Roadmap for Change
While individual sessions follow a predictable structure, the overall course of therapy requires comprehensive treatment planning. A treatment plan is a structured document that outlines the client’s presenting problems, diagnosis (if applicable), therapeutic goals, specific objectives, planned interventions, and methods for measuring progress. Treatment planning typically begins after the initial assessment and may be revised as therapy progresses.
Effective treatment plans are collaborative. Rather than the therapist imposing goals on the client, both parties work together to identify what the client wants to achieve and how they will get there. This collaboration increases client motivation and investment in the therapeutic process. When clients feel ownership of their goals, they are more likely to work actively toward achieving them.
SMART Goals: Making Objectives Measurable
One of the most important elements of treatment planning is setting SMART goals. SMART is an acronym that stands for:
Specific: goals should be clear and well-defined, not vague. Instead of “feel better,” a specific goal might be “reduce panic attacks.”
Measurable: goals should be quantifiable so that progress can be tracked. For example, “reduce panic attacks from 5 per week to 1 per week” is measurable.
Achievable: goals should be realistic given the client’s resources, abilities, and circumstances. Setting impossibly difficult goals sets clients up for failure.
Relevant: goals should align with the client’s values, needs, and overall life situation. They should matter to the client personally.
Time-bound: goals should have a specific timeframe. “Within 12 weeks” or “by the end of treatment” creates urgency and allows for evaluation.
For example, a vague goal like “improve mood” becomes a SMART goal when reframed as: “Within 8 weeks, reduce depression symptoms (as measured by the PHQ-9: Patient Health Questionnaire-9)) from a score of 18 to below 10 through weekly therapy sessions and daily behavioural activation exercises.”
Treatment plans distinguish between goals (the broader aims of treatment) and objectives (the specific steps needed to achieve those goals). A goal might be “reduce social anxiety,” while objectives would include “learn and practice relaxation techniques within the first four sessions” and “engage in one social situation per week using coping strategies learned in therapy.”
The treatment plan also specifies interventions — the therapeutic techniques and approaches that will be used to help the client reach their objectives. Interventions might include cognitive restructuring, exposure therapy, mindfulness practice, family therapy sessions, or emotion regulation skills training. The choice of interventions depends on the client’s diagnosis, goals, and the therapist’s theoretical orientation and training.
Measuring Progress and Outcomes
How do therapists and clients know if therapy is working? Outcomes refer to the results of therapeutic intervention — the changes that occur in the client’s symptoms, functioning, and well-being. Measuring outcomes is essential for evaluating treatment effectiveness and making adjustments when needed.
Many therapists use standardized outcome measures or assessment scales to track progress systematically. For depression, the PHQ-9 provides a numerical score that can be tracked over time. For anxiety, the GAD-7 (Generalized Anxiety Disorder-7) serves a similar purpose. When a client’s score decreases from 20 to 8 over the course of treatment, both therapist and client have concrete evidence that therapy is working.
Progress is also measured through regular check-ins during sessions. Therapists might ask, “Are you noticing any changes?” or “How are you managing the situations that used to trigger your anxiety?” Client self-reports of improved mood, better relationships, or increased coping abilities all indicate positive outcomes.
Termination and Relapse Prevention
All therapy relationships eventually end, and termination — the planned conclusion of therapy — is an important phase that requires careful attention. Termination is appropriate when clients have achieved their treatment goals, learned skills for managing their difficulties, and feel ready to continue their progress independently.
Effective termination is not abrupt. Therapists typically begin discussing termination several sessions before the final meeting, giving clients time to process their feelings about ending therapy and to consolidate their gains. The termination phase includes reviewing progress, celebrating achievements, and acknowledging the relationship that has developed.
A crucial component of termination is relapse prevention planning. While clients may have made significant progress during therapy, they remain vulnerable to returning to old patterns when faced with stress or new challenges. Relapse prevention involves helping clients identify their warning signs, develop strategies for managing future difficulties, and create a plan for what to do if symptoms return.
Relapse prevention planning might include: identifying high-risk situations that could trigger old patterns; reviewing coping strategies learned in therapy; creating a written plan for managing warning signs; discussing when to seek additional therapy in the future; and ensuring clients feel confident in their ability to maintain their gains.
Research shows that structured therapies that include explicit relapse prevention planning help clients maintain their improvements long after therapy ends. By preparing clients for potential challenges and giving them tools to manage independently, therapists set them up for lasting success.
From the structured framework of individual sessions to the comprehensive roadmap of treatment planning, effective psychotherapy balances organization with flexibility, always keeping the client’s goals and well-being at the center of the work.
Comprehension questions:
1. What is the “therapeutic frame” and why is it important?
2. What happens during the check-in at the beginning of a session?
3. What is agenda setting and why is it collaborative?
4. What is the purpose of homework in therapy?
5. What does SMART stand for in SMART goals?
6. What is the difference between goals and objectives in a treatment plan?
7. How can therapists measure whether therapy is working?
8. When is termination appropriate?
9. What is relapse prevention and why is it important?
10. Give an example of a SMART goal for a client with depression.
VOCABULARY:
Treatment Planning and SMART Goals Terminology
A. Find words in the text that match these definitions:
1. The consistent boundaries and structure that provide safety in therapy (paragraph 2): _______
2. A brief opening discussion about the client’s current state (paragraph 4): _______
3. Process where therapist and client decide what to focus on during session (paragraph 5): _______
4. The main part of the session where therapeutic work happens (paragraph 6): _______
5. Therapeutic tasks that help clients practice between sessions (paragraph 7): _______
6. A structured document outlining problems, goals, and interventions (paragraph 9): _______
7. Tools or techniques used to help clients achieve their objectives (paragraph 14): _______
8. The results of therapeutic intervention (paragraph 15): _______
9. The planned conclusion of therapy (paragraph 17): _______
10. Strategies to help clients maintain gains and avoid returning to old patterns (paragraph 19): _______
B. Complete the collocations from the text:
1. therapeutic _______
2. check-_______
3. agenda _______
4. homework _______
5. treatment _______
6. SMART _______
7. measurable _______
8. relapse _______
9. outcome _______
10. session _______
C. Word families
Complete the table:
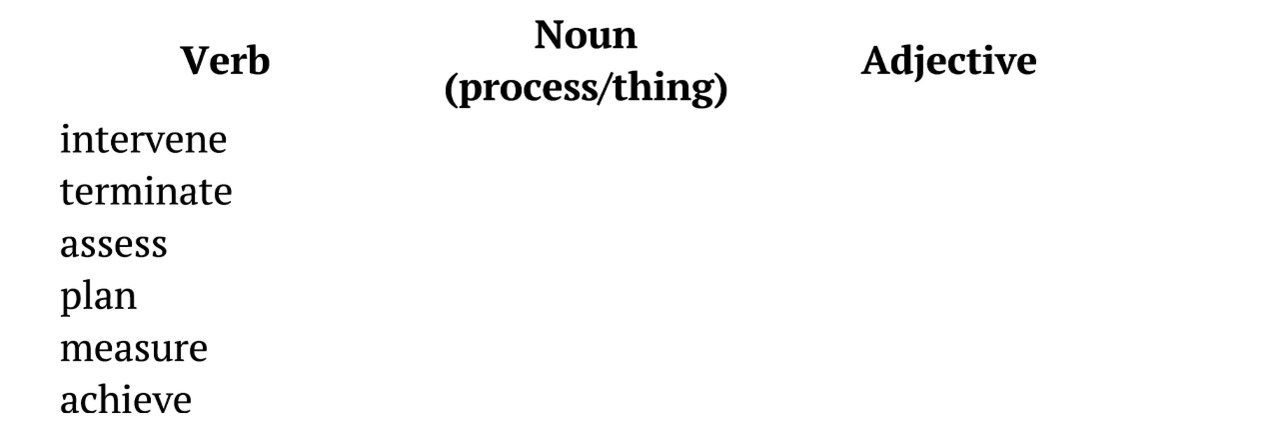
Discussion questions:
1. How structured should therapy sessions be?
2. Why is it important for clients to participate in setting their own goals?
3. What should a therapist do if a client doesn’t complete homework assignments?
4. How can therapists balance following a treatment plan with being responsive to clients’ immediate needs?
5. Should all therapy have a planned ending, or can it continue indefinitely?
6. What are the risks of not having a relapse prevention plan?
GRAMMAR FOCUS:
Future Simple, “going to,” and Present Continuous for Plans and Timelines
When discussing treatment plans, session structure, and therapeutic goals, we use different future forms depending on the type of plan or prediction.
A. Future Simple (will + main verb)
Use: predictions, spontaneous decisions, promises, and general future facts
Form:
• Affirmative: Subject + will + main verb
• Negative: Subject + will not (won’t) + main verb
• Questions: Will + subject + main verb?
Examples from therapy:
• This intervention will help you manage anxiety better.
• Therapy will take approximately 12–16 sessions.
• The therapist will review your progress regularly.
• I will support you throughout this process.
• These coping skills will be useful in stressful situations.
B. “Going to” + main verb
Use: planned intentions, decisions already made, and predictions based on present evidence
Form:
• Affirmative: Subject + am/is/are + going to + main verb
• Negative: Subject + am/is/are + not + going to + main verb
• Questions: Am/Is/Are + subject + going to + main verb?
Examples from therapy:
• We are going to work on your communication skills.
• I am going to assign homework to practise between sessions.
• The client is going to keep a thought diary this week.
• We are going to focus on relapse prevention in our final sessions.
• They are going to terminate therapy after achieving their goals.
C. Present Continuous for arrangements
Use: fixed arrangements and scheduled appointments
Form:
• Affirmative: Subject + am/is/are + main verb-ing
• Negative: Subject + am/is/are + not + main verb-ing
• Questions: Am/Is/Are + subject + main verb-ing?
Examples from therapy:
• We are meeting next Tuesday at 3 PM.
• I am seeing my therapist this week.
• The client is coming for their intake session tomorrow.
• We are having our termination session next month.
• They are not attending group therapy this week.
Exercise 1: Choose the correct form
Complete the sentences with the correct future form of the verb in brackets:
1. In our next session, we _______ (explore) your childhood experiences.
2. I think this treatment plan _______ (be) effective for your symptoms.
3. We _______ (meet) every Wednesday at 4 PM for the next three months.
4. The therapist _______ (use) CBT techniques to address your negative thoughts.
5. Look at your progress! You _______ (achieve) your goals soon.
6. I _______ (assign) you homework to practise assertiveness skills.
7. Our termination session _______ (take place) on December 15th.
8. This relapse prevention plan _______ (help) you maintain your progress.
Exercise 2: Will vs. Going to
Decide if each sentence should use “will” or “going to”:
1. A: I haven’t decided which intervention to use yet.
B: I _______ (recommend) trying cognitive restructuring first.
2. We _______ (start) working on your social anxiety in today’s session. (This was planned last week)
3. A: The client seems very distressed.
B: Don’t worry. I _______ (check in) with him right away. (spontaneous decision)
4. According to the treatment plan, therapy _______ (last) for 16 weeks.
5. I can see you’re making great progress. You _______ (reach) your goals very soon. (based on evidence)
Exercise 3: Complete the treatment plan discussion
Complete this dialogue between a therapist and client using appropriate future forms:
Therapist: So, we _______ (work) together for approximately 12 sessions. In our first few sessions, we _______ (focus) on assessment and goal-setting.
Client: That sounds good. What _______ (happen) in the later sessions?
Therapist: We _______ (use) various CBT techniques to help you manage your anxiety. I _______ (teach) you relaxation skills and cognitive restructuring.
Client: _______ (I / have) homework?
Therapist: Yes, I _______ (assign) practice exercises between sessions. This _______ (help) you apply what we learn in therapy to your daily life.
Client: When _______ (we / meet)?
Therapist: We _______ (meet) every Thursday at 2 PM. Does that work for you?
Client: Perfect. I _______ (see) you next Thursday, then!
Exercise 4: Correct the mistakes
Find and correct the mistakes in these sentences:
1. We will meeting for our session tomorrow at 3 PM.
2. I think the client is going achieve their goals soon.
3. The therapist going to assign homework next week.
4. Our final session will taking place in June.
5. What we are going to work on today?
6. The treatment plan are going to include relaxation techniques.
7. I meet my supervisor next Monday to discuss this case.
8. Will the client going to attend group therapy?
COMMUNICATION:
A Therapeutic Session: Setting Goals and Creating a Treatment Plan
Context: This is session 3. The client, James, is a 37-year-old professional who came to therapy for anxiety and sleep problems. He has been in therapy for three weeks. The therapist is Dr. Roberts.
Dr. Roberts: Good morning, James. How have you been since we last met?
James: Hi, Dr. Roberts. I’ve been… okay, I guess. Better than before I started therapy, but I still have difficult days.
Dr. Roberts: I’m glad to hear there’s been some improvement. Can you tell me a bit more about the difficult days? What makes them challenging?
James: Well, I still feel overwhelmed at work quite often. And I’m having trouble sleeping — my mind just won’t switch off at night.
Dr. Roberts: I understand. These seem like important things to address. Today, I’d like us to work on something specific — creating clear treatment goals and developing a plan for our work together. Does that sound good to you?
James: Yes, definitely. I think I need that. Sometimes I’m not sure what we’re working towards.
Dr. Roberts: That’s very honest of you, and it’s exactly why setting goals is so important. Let’s start with what you’d like to change. If our therapy together is successful, what would be different in your life?
James: I want to feel less anxious, especially at work. And I want to sleep better. Also… I’d like to feel more confident in general.
Dr. Roberts: Those are great starting points. Let’s work on making them more specific so we can track your progress. You mentioned feeling less anxious at work — can you describe what that would look like in practical terms?
James: I suppose… I’d be able to present at team meetings without my heart racing. And I wouldn’t spend my lunch breaks worrying about what might go wrong in the afternoon.
Dr. Roberts: Excellent. So, one goal could be about managing anxiety in specific work situations. Let’s make it even more concrete. How often do you present at meetings currently?
James: About once a week, usually on Fridays.
Dr. Roberts: And how would you rate your anxiety level during these presentations right now, from 0 to 10, where 0 means no anxiety at all and 10 means extreme anxiety?
James: Probably an 8 or 9. It’s really high.
Dr. Roberts: Okay. So, let’s create a SMART goal — that means it’s Specific, Measurable, Achievable, Relevant, and Time-bound. How does this sound: “Within 10 weeks, I will present at weekly team meetings and reduce my anxiety level from 8/10 to 4/10, measured before and during the presentation.”
James: That sounds… challenging but possible, I think.
Dr. Roberts: Good. It should feel like a stretch but not impossible. Now, what about sleep? What would better sleep look like for you?
James: Falling asleep within 30 minutes instead of lying awake for two hours. And maybe waking up feeling rested, not exhausted.
Dr. Roberts: How many nights per week are you having trouble sleeping currently?
James: Five or six nights. It’s pretty consistent.
Dr. Roberts: Alright. Here’s a possible goal: “Within 8 weeks, I will fall asleep within 30 minutes on at least 5 nights per week by practicing sleep hygiene techniques and relaxation exercises.”
James: That would make such a difference to my life.
Dr. Roberts: I believe it will. Now, you also mentioned confidence. That’s a bit broader. Can you give me an example of a situation where you’d like to feel more confident?
James: Social situations, I think. I avoid going out with friends because I worry I’ll say something stupid or that people won’t like me.
Dr. Roberts: How often are you declining social invitations right now?
James: Almost always. I probably say no nine times out of ten.
Dr. Roberts: And realistically, how often would you like to be able to say yes?
James: Maybe… half the time? At least at first.
Dr. Roberts: That’s a realistic target. So, our third goal might be: “Within 12 weeks, I will accept and attend at least 50% of social invitations I receive, with a minimum of two social events per month.”
James: Okay. These goals make it all feel more… real. More manageable.
Dr. Roberts: That’s exactly the purpose. Now let’s talk about how we’re going to help you achieve these goals. Based on what you’ve told me over our sessions, I think Cognitive behavioural Therapy would be very effective for you. Do you know anything about CBT?
James: Not really. What does it involve?
Dr. Roberts: CBT focuses on the connection between your thoughts, feelings, and behaviours. We’ll identify unhelpful thinking patterns that increase your anxiety and work on developing more balanced, realistic thoughts. We’ll also use exposure exercises to gradually help you face situations you’re avoiding.
James: Exposure exercises? That sounds scary.
Dr. Roberts: It will be gradual and at your pace. For example, we might start with smaller social situations before working up to bigger ones. And we’ll teach you coping strategies first — like relaxation techniques and thought challenging — so you have tools to manage the anxiety.
James: Okay. That sounds more manageable.
Dr. Roberts: Good. So, here’s our treatment plan: We’ll meet weekly for approximately 12–14 sessions. Each session, we’ll check on your progress, review any homework exercises, learn and practice new skills, and plan what to work on between sessions. For your work anxiety, we’ll use thought records to identify and challenge anxious thoughts. For sleep, we’ll implement a sleep hygiene plan and teach you progressive muscle relaxation. And for social confidence, we’ll create an exposure hierarchy — starting with less anxiety-provoking situations and gradually building up.
James: And the homework you mentioned — what would that involve?
Dr. Roberts: Between sessions, you’ll practice the skills we work on here. For example, keeping thought records, practicing relaxation exercises daily, or gradually completing exposure tasks. The homework is where most of the change happens — our sessions are for learning and planning, but you’ll do the real work outside this room.
James: That makes sense. I’m nervous but I’m ready to try.
Dr. Roberts: That’s a great attitude. Remember, we’ll review your progress regularly. Every few sessions, we’ll check whether these goals still feel relevant and whether we need to adjust them. This plan isn’t set in stone — it’s a working document we’ll adapt as needed. How are you feeling about everything we’ve discussed?
James: Honestly? A bit overwhelmed, but also relieved. It’s good to have a clear direction.
Dr. Roberts: That’s a very normal reaction. For next week, I’d like you to start monitoring your anxiety and sleep patterns. I’m going to give you a simple diary sheet where you can record your anxiety levels in different situations and note what time you go to bed and fall asleep each night. This will give us baseline data and help you become more aware of patterns.
James: Okay, I can do that.
Dr. Roberts: Excellent. Let’s summarize what we’ve agreed today. We’ve set three main goals: reducing your anxiety at work presentations to 4/10 within 10 weeks, improving your sleep by falling asleep within 30 minutes at least 5 nights per week within 8 weeks, and accepting 50% of social invitations within 12 weeks. We’ll use CBT techniques including thought records, relaxation exercises, and gradual exposure. Does that sound right?
James: Yes, that covers it.
Dr. Roberts: How helpful was today’s session for you?
James: Very helpful. I feel like I understand what we’re doing now and where we’re headed.
Dr. Roberts: I’m glad to hear that. I’ll see you next week, at the same time. And remember to bring your anxiety and sleep diary.
TASK 1: True / False / Not Mentioned
Read the statements below about the therapeutic session. Decide if each statement is:
• TRUE — the statement agrees with the information
• FALSE — the statement contradicts the information
• NOT MENTIONED — the information is not given
Statements:
1. This is James’s first therapy session with Dr. Roberts.
2. James is having difficulty sleeping because his mind won’t switch off at night.
3. Dr. Roberts plans to use Cognitive behavioural Therapy with James.
4. James currently rates his anxiety during presentations as 8 or 9 out of 10.
5. James has been diagnosed with panic disorder.
6. James accepts most social invitations he receives.
7. The treatment plan includes approximately 12–14 weekly sessions.
8. Dr. Roberts will adjust the treatment plan if needed as therapy progresses.
9. James needs to practice relaxation exercises twice a day.
10. Dr. Roberts assigns James an anxiety and sleep diary for homework.
ㅤ
TASK 2: Answer the Questions
1. How is James feeling compared to before he started therapy?
2. What are the three main issues James wants to address in therapy?
3. What does SMART stand for in goal-setting?
4. What is James’s first SMART goal about work presentations?
5. How often is James currently having trouble sleeping?
6. What percentage of social invitations does James want to be able to accept?
7. What three main techniques will Dr. Roberts use to help James?
8. What is James’s homework assignment for next week?
ㅤ
TASK 3: Personal Response
Discuss:
1. James feels “overwhelmed but also relieved” after setting goals. Why do you think clear goals can create both feelings at the same time?
2. Dr. Roberts says, “The homework is where most of the change happens.” Do you agree that practice outside therapy sessions is more important than the sessions themselves? Why or why not?
3. One of James’s goals is to attend at least two social events per month. Do you think this is realistic for someone with social anxiety? Would you set the goal higher or lower?
TASK 4: Role Play
Work in pairs. One person is a psychotherapist, the other is a client.
The client presents with:
• Chronic stress from work overload
• Frequent headaches and muscle tension
• Difficulty saying “no” to additional responsibilities
• Feeling burned out and exhausted
The psychotherapist should:
• Ask questions to understand the client’s difficulties
• Help the client formulate 2–3 SMART goals
• Suggest appropriate interventions (e.g., stress management techniques, assertiveness training, relaxation exercises)
• Assign homework for the coming week
• Summarize the treatment plan
Time: 10—15 minutes
After the role play, discuss:
• Was it easy or difficult to create SMART goals?
• Did the goals feel realistic and achievable?
• What interventions seemed most appropriate for this client’s problems?
PROFESSIONAL PRACTICE:
Creating Effective Treatment Plans
Sample Treatment Plans
Treatment Plan 1: Depression
Client: 32-year-old female with major depressive disorder
Presenting Problems: Low mood, loss of interest in activities, difficulty concentrating, sleep disturbance
Treatment Approach: Cognitive-behavioural Therapy
Goal: Reduce depressive symptoms and improve daily functioning within 12 weeks
SMART Objectives:
1. Within 4 weeks, client will identify and challenge 3 negative automatic thoughts daily using thought records
2. By week 6, client will engage in 3 pleasurable activities per week (behavioural activation)
3. By week 12, client will score below 10 on PHQ-9* (currently 18)
Interventions:
• Cognitive restructuring
• behavioural activation
• Sleep hygiene psychoeducation
• Homework assignments (thought records, activity scheduling)
Outcome Measures: PHQ-9 administered every 3 sessions
Planned Duration: 12–16 weekly sessions
Relapse Prevention: Identify warning signs, maintain activity schedule, know when to seek additional support
* PHQ-9 (Patient Health Questionnaire-9) — Опросник здоровья пациента-9
Treatment Plan 2: Social Anxiety
Client: 25-year-old male with social anxiety disorder
Presenting Problems: Fear of judgment, avoidance of social situations, physical anxiety symptoms
Treatment Approach: Cognitive-behavioural therapy with exposure
Goal: Decrease social anxiety and increase participation in social activities within 16 weeks
SMART Objectives:
1. Within 4 weeks, learn and practise relaxation techniques with 80% success rate
2. By week 8, attend one low-anxiety social situation per week using coping strategies
3. By week 12, give a presentation at work (previously avoided)
4. By week 16, report anxiety in social situations decreased from 8/10 to 3/10
Interventions:
• Cognitive restructuring of social anxiety thoughts
• Progressive muscle relaxation training
• Graduated exposure hierarchy
• Social skills practice
• Homework: weekly exposure exercises
Outcome Measures: GAD-7*, subjective anxiety ratings, behavioural tracking
Planned Duration: 16 weekly sessions
Relapse Prevention: Continued gradual exposures, recognition of anxiety warning signs, maintenance of coping strategies
*GAD-7 (Generalized Anxiety Disorder-7) – стандартизированный опросник из 7 вопросов для скрининга и оценки тяжести генерализованного тревожного расстройства
Useful Phrases for Treatment Planning
Describing Presenting Problems:
• The client presents with…
• Primary concerns include…
• The client reports experiencing…
• Main difficulties are…
Setting Goals:
• The overall goal of treatment is to…
• The client aims to…
• We will work toward…
• Treatment will focus on…
Writing SMART Objectives:
• Within [timeframe], the client will…
• By [date], the client will be able to…
• The client will demonstrate… [number] times per [period]
• By the end of treatment, the client will achieve…
Describing Interventions:
• Treatment will include…
• Therapeutic techniques will consist of…
• We will utilize…
• The approach combines…
• Sessions will incorporate…
Measuring Outcomes:
• Progress will be measured using…
• We will track…
• Outcome measures include…
• Success will be indicated by…
Planning Termination:
• Termination is planned for…
• Treatment will conclude when…
• We will begin discussing termination…
• Relapse prevention will include…
Practice Exercises
Exercise 1: Identify SMART Elements
Look at these goals and identify which SMART criteria each one meets or lacks:
1. “Client will feel better”
2. “Within 8 weeks, client will practise relaxation exercises 5 times per week”
3. “Client will reduce panic attacks from 5 per week to 1 per week within 10 weeks as measured by daily tracking”
Exercise 2: Convert Vague Goals to SMART Goals
Rewrite these vague goals as SMART goals:
1. Vague: Client will have less anxiety
SMART: _________________________________
2. Vague: Client will improve relationships
SMART: _________________________________
3. Vague: Client will cope better with stress
SMART: _________________________________
Exercise 3: Match Interventions to Goals
Match each goal with the most appropriate intervention:
Goals:
1. Reduce frequency of panic attacks
2. Improve communication with a partner
3. Decrease depressive symptoms
4. Manage anger more effectively
Interventions:
a) behavioural activation and cognitive restructuring
b) Couples therapy and active listening skills training
c) Interoceptive exposure and breathing techniques
d) Anger management techniques and cognitive reappraisal
Exercise 4: Create a Session Structure
You are meeting a client for the third time. They have been practising thought records as homework. Create an outline for today’s session including:
• Check-in: _________________________________
• Agenda setting: _________________________________
• Working section: _________________________________
• Summary: _________________________________
• Homework: _________________________________
Exercise 5: Write a Mini Treatment Plan
Create a brief treatment plan for this scenario:
Client: 28-year-old female experiencing work-related stress, sleep problems, and difficulty saying “no” to extra responsibilities
Your treatment plan should include:
• One overall goal
• Two SMART objectives
• Three specific interventions
• One outcome measure
• Planned duration
Exercise 6: Relapse Prevention Planning
A client with depression has achieved their treatment goals and will terminate therapy in two sessions. List 5 elements you would include in their relapse prevention plan:
1. _________________________________
2. _________________________________
3. _________________________________
4. _________________________________
5. _________________________________
Vocabulary and Collocations for Unit 4
check-in — проверка состояния, начальное обсуждение
agenda setting — установление повестки дня
treatment plan — план лечения
SMART goals — СМАРТ-цели
intervention — вмешательство/интервенция
termination — завершение терапии
relapse prevention — профилактика рецидива
homework — домашнее задание
building rapport — выстраивание раппорта
gathering history — сбор анамнеза
setting initial goals — постановка начальных целей
therapeutic process — терапевтический процесс
regular sessions — регулярные сессии
homework review — обзор домашнего задания
reviewing progress — обзор прогресса
relapse prevention planning — планирование профилактики рецидива
measuring progress — измерение прогресса
therapeutic frame — терапевтические рамки (сеттинг)
session structure — структура сессии
consistent boundaries — устойчивые границы
confidentiality agreements — соглашения о конфиденциальности
current state — текущее состояние
experiences since the last meeting — переживания после последней встречи
significant events — значимые события
present moment — настоящий момент
immediate emotional state — непосредственное эмоциональное состояние
urgent issue — срочная проблема
immediate attention — первоочередное внимание
collaborative process — совместный процесс
most pressing concerns — самые актуальные проблемы
working section — рабочая секция
therapeutic techniques — терапевтические техники
negative automatic thoughts — негативные автоматические мысли
unconscious patterns — бессознательные паттерны
transference — перенос
closing and summary — завершение и резюме
key insights — ключевые инсайты
homework assignment — назначение домашнего задания
therapeutic tasks — терапевтические задачи
thought diary — дневник мыслей
relaxation techniques — техники релаксации
real-life situation — реальная жизненная ситуация
complete homework assignments — выполнять домашние задания
make faster progress — ускорить прогресс
achieve better outcomes — достигать лучших результатов
comprehensive treatment planning — всестороннее планирование лечения
presenting problems — предъявляемые проблемы
diagnosis — диагноз
therapeutic goals — терапевтические цели
specific objectives — конкретные цели
planned interventions — запланированные вмешательства/интервенции
measuring progress — измерение прогресса
initial assessment — первичная оценка
client motivation — мотивация клиента
investment in the therapeutic process — вовлеченность в терапевтический процесс
specific — конкретный
measurable — измеримый
achievable — достижимый
relevant — релевантный
time-bound — ограниченный по времени
reduce panic attacks — снизить панические атаки
vague goal — расплывчатая цель
broader aims — более широкие цели
treatment goals — цели лечения
objectives — задачи
specific steps — конкретные шаги
reduce social anxiety — снизить социальную тревожность
learn and practise — изучать и практиковать
coping strategies — стратегии совладания
engage in — участвовать в
cognitive restructuring — когнитивная реструктуризация
exposure therapy — экспозиционная терапия
mindfulness practice — практика осознанности
family therapy sessions — сеансы семейной терапии
emotion regulation skills — навыки эмоциональной регуляции
theoretical orientation — теоретическая ориентация
outcomes — результаты
therapeutic intervention — терапевтическое вмешательство
treatment effectiveness — эффективность лечения
standardized outcome measures — стандартизированные методики оценки результата
assessment scales — оценочные шкалы
track progress systematically — отслеживать прогресс систематически
PHQ-9 (Patient Health Questionnaire-9) — PHQ-9 (Опросник здоровья пациента-9)
GAD-7 (Generalized Anxiety Disorder-7) — GAD-7 (Опросник: Генерализованное тревожное расстройство-7)
numerical score — числовая оценка/числовой рейтинг
concrete evidence — конкретное доказательство
regular check-ins — регулярные проверки
client self-reports — самоотчеты клиента
improved mood — улучшенное настроение
better relationships — более хорошие отношения
increased coping abilities — улучшенные навыки совладания
positive outcomes — позитивные результаты
planned conclusion — запланированное завершение
achieved treatment goals — достигнутые цели лечения
learned skills — освоенные навыки
independently — самостоятельно/независимо
effective termination — эффективное завершение
abrupt — резкий
process feelings — обрабатывать чувства
consolidate gains — закреплять достижения
celebrating achievements — празднование достижений
acknowledging the relationship — осознание отношений (в терапии)
warning signs — предупреждающие знаки
returning to old patterns — возвращение к старым паттернам
high-risk situations — ситуации высокого риска
trigger old patterns — запускать старые паттерны (поведения)
written plan — письменный план
seek additional therapy — обратиться за дополнительной терапией
maintain gains — поддерживать достижения
structured therapy — структурированная терапия
explicit relapse prevention planning — явное планирование профилактики рецидива
maintain improvements — поддерживать улучшения
lasting success — длительный успех
baseline data — исходные данные
sleep hygiene — гигиена сна
progressive muscle relaxation — прогрессивная мышечная релаксация
exposure hierarchy — иерархия экспозиции
thought records — записи мыслей
behavioural activation — поведенческая активация
depression symptoms — симптомы депрессии
daily functioning — повседневное функционирование
major depressive disorder — большое депрессивное расстройство
low mood — пониженное настроение
loss of interest — потеря интереса
difficulty concentrating — трудности с концентрацией
sleep disturbance — нарушение сна
pleasurable activities — приятные занятия/виды деятельности
social anxiety disorder — социальное тревожное расстройство
fear of judgment — страх осуждения
avoidance of social situations — избегание социальных ситуаций
physical anxiety symptoms — физические симптомы тревоги
low-anxiety social situation — малотревожная социальная ситуация
subjective anxiety ratings — субъективные оценки тревоги
behavioural tracking — поведенческое отслеживание
continued gradual exposures — продолжающиеся постепенные экспозиции
recognition of warning signs — распознавание предупреждающих знаков
maintenance of coping strategies — поддержание стратегий совладания
UNIT 5.
MAJOR SKILLS OF A PSYCHOLOGIST
LEAD-IN:
Professional Skills and Competencies
Activity 1: What makes an effective psychologist?
Read the list of professional skills below. Think about each skill and complete the tasks:
Professional skills:
• Active listening — understanding what the client really means
• Building rapport — creating trust with clients
• Ethical decision-making — knowing what is right in difficult situations
• Teamwork — collaborating with other professionals
• Assessment skills — gathering and analyzing information about clients
• Cultural sensitivity — working with people from different backgrounds
Tasks:
1. Number the skills from 1 to 6 (1 = most important, 6 = least important for you)
2. Circle TWO skills you already have
3. Underline ONE skill you want to develop further
Be ready to explain your choices.
Activity 2: Skills brainstorm
Work in small groups. You have 3 minutes to write down as many professional skills as you can that psychologists need in their practice.
Example: active listening, assessment, empathy, critical thinking, communication skills…
Activity 3: Discussion questions
Discuss these questions with your partner:
1. What do you think are the three most important skills for a psychologist?
2. Are some skills more important in certain settings (hospital vs. private practice)?
3. Can all professional skills be taught, or are some innate?
4. What’s the difference between clinical skills and interpersonal skills?
5. How do psychologists maintain their professional boundaries?
6. What role does research play in psychological practice?
ㅤ
Key vocabulary for this unit:
ㅤ
Match the words with their definitions:
1. Competency
2. Assessment
3. Intervention
4. Case formulation
5. Professional boundaries
6. Clinical judgment
7. Ethical decision-making
ㅤ
a) The ability to make informed professional decisions based on evidence and experience
b) The process of gathering and evaluating information about a client’s psychological state
c) Clear limits that protect both psychologist and client in the professional relationship
d) A specific skill or ability required for professional practice
e) Making choices that align with professional ethical codes and standards
f) An action or treatment designed to help resolve a psychological problem
g) A comprehensive understanding of a client’s problems, their causes, and maintaining factors
READING:
Essential Competencies for Psychological Practice
Pre-reading task
Before you read, discuss:
1. What core competencies do you think all psychologists need?
2. How is “competency” different from “skill”?
3. Why might competencies vary across different psychology settings?
4. How do psychologists develop and maintain their competencies?
Essential Competencies for Psychological Practice
Professional psychology requires a complex set of competencies that enable psychologists to work effectively with diverse clients, make sound professional judgments, and provide evidence-based services. While specific competencies may vary depending on the area of psychology practice, certain core competencies are fundamental to all psychological work.
Interpersonal and Relationship Skills
The foundation of effective psychological practice is the ability to establish and maintain professional relationships. This competency encompasses more than simple communication — it involves creating a therapeutic alliance built on trust, respect, and genuine understanding. Psychologists must be able to work with clients from diverse backgrounds, adapting their interpersonal style to meet individual needs while maintaining professional boundaries.
Effective relationship skills include active listening, empathic understanding, and the ability to create a safe, non-judgmental environment. A psychologist should be able to establish rapport quickly, recognize both verbal and non-verbal communication, and respond sensitively to clients’ emotional states. These skills also extend to professional relationships with colleagues, requiring psychologists to collaborate effectively in multidisciplinary teams and consult appropriately with other professionals.
Assessment and Evaluation Competencies
Assessment is a core competency that distinguishes psychological practice from other helping professions. Psychologists must possess advanced knowledge of assessment methods, measurement theory, and diagnostic frameworks. This competency involves selecting appropriate assessment tools, conducting clinical interviews, administering psychological tests, and integrating multiple sources of information to form comprehensive conclusions.
Effective assessment requires critical thinking and analytical skills. A psychologist should be able to gather relevant information through various methods — interviews, observations, standardized tests, and behavioural assessments. They must understand the strengths and limitations of different assessment approaches and select methods appropriate to the client’s age, cultural background, and presenting concerns. The assessment process should lead to case formulation: a comprehensive understanding of the client’s problems, contributing factors, and potential intervention strategies.
Psychologists ought to interpret assessment data within appropriate theoretical frameworks, considering biological, psychological, and social factors. They must be able to communicate findings clearly to clients, families, and other professionals, translating technical information into understandable language.
Intervention and Treatment Skills
Intervention competency encompasses the knowledge and skills needed to implement effective psychological treatments. This includes understanding various therapeutic approaches, selecting evidence-based interventions appropriate to the client’s needs, and implementing treatment plans effectively. Psychologists should possess detailed knowledge of intervention techniques relevant to their practice areas and be able to adapt these methods to individual circumstances.
Effective intervention requires ongoing monitoring and evaluation. A psychologist must regularly assess treatment progress, modify interventions when necessary, and demonstrate flexibility in their approach. They should be able to identify when interventions are not working and be willing to try alternative strategies or refer clients to other professionals when appropriate.
Intervention skills also include crisis management, the ability to work with resistance, and competence in addressing complex presentations. Psychologists might need to integrate multiple therapeutic approaches and should be able to explain their treatment decisions based on evidence and clinical judgment.
Professional Communication and Consultation
Professional communication extends beyond client interactions to include documentation, report writing, consultation with colleagues, and collaboration with other professionals. Psychologists must maintain clear, accurate clinical records that document assessment findings, treatment plans, progress notes, and outcomes. Written communication should be professional, comprehensive, and compliant with legal and ethical standards.
Consultation competency involves the ability to provide psychological expertise to other professionals, organizations, and systems. A psychologist should be able to explain psychological concepts clearly, offer evidence-based recommendations, and collaborate effectively in multidisciplinary settings. They must understand their professional role in relation to other disciplines and know when to seek consultation from colleagues or specialists.
Effective professional communication requires cultural sensitivity and the ability to adapt communication style to different audiences. Psychologists ought to communicate assessment results and treatment recommendations in ways that clients and other stakeholders can understand and use.
Ethical Decision-Making and Professional Judgment
Ethical competence is fundamental to all psychological practice. Psychologists must possess thorough knowledge of professional ethics codes, legal requirements, and standards of practice. More importantly, they need the ability to apply ethical principles to complex real-world situations where guidelines may be unclear or competing values are at stake.
Ethical decision-making involves recognizing ethical issues when they arise, analyzing dilemmas from multiple perspectives, consulting relevant resources and colleagues, and making informed decisions. Psychologists must maintain professional boundaries, manage multiple relationships appropriately, and protect client welfare while respecting autonomy.
Clinical judgment — the ability to make sound professional decisions based on evidence, experience, and contextual factors — is closely related to ethical competence. Good clinical judgment requires integrating theoretical knowledge, research evidence, assessment data, and understanding of the individual client. Psychologists should be able to recognize the limits of their competence and practice within appropriate boundaries.
Research and Evidence-Based Practice
Contemporary psychology practice must be grounded in scientific evidence. Psychologists should possess research literacy — the ability to access, critically evaluate, and apply research findings to their practice. This competency includes understanding research methods, interpreting statistical analyses, and staying current with developments in relevant areas.
Evidence-based practice requires psychologists to integrate the best available research with clinical expertise and client preferences. Practitioners should be able to evaluate the quality of research evidence, understand what interventions have empirical support for specific conditions, and apply this knowledge to individual cases. Many psychologists also contribute to the research mainly through their own investigations, outcome evaluations, or participation in research projects.
Reflective Practice and Professional Development
Бесплатный фрагмент закончился.
Купите книгу, чтобы продолжить чтение.